Radioablation in calcaneal osteoid osteoma – Resection and reconstruction technique with autologous graft
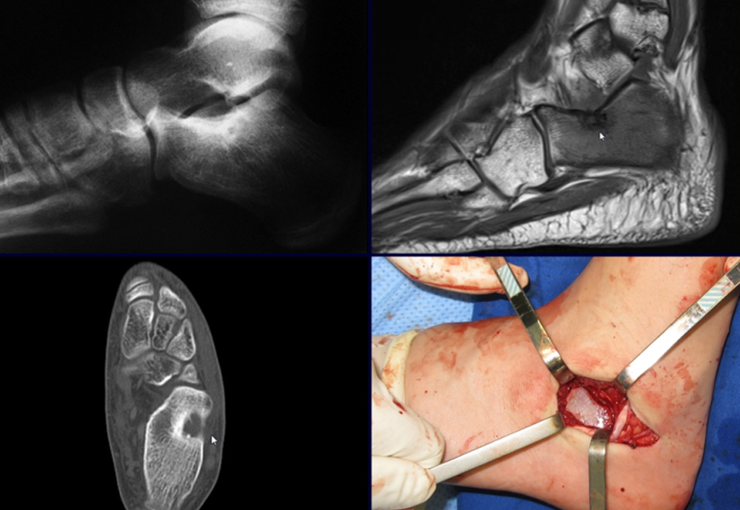
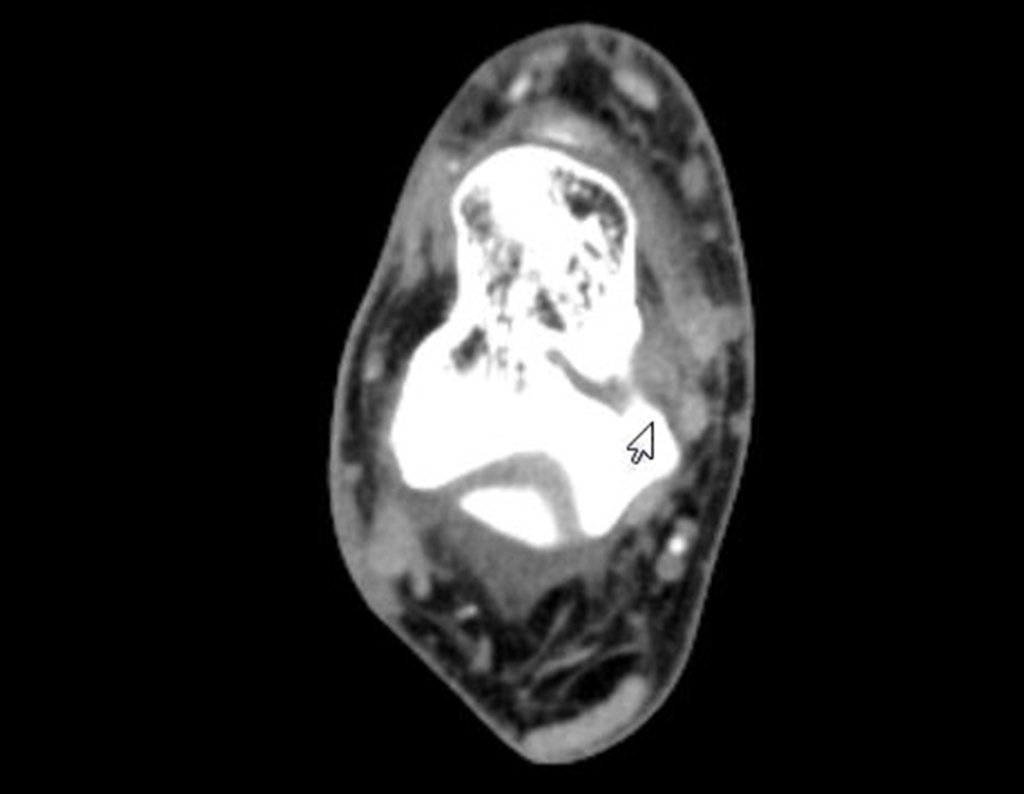
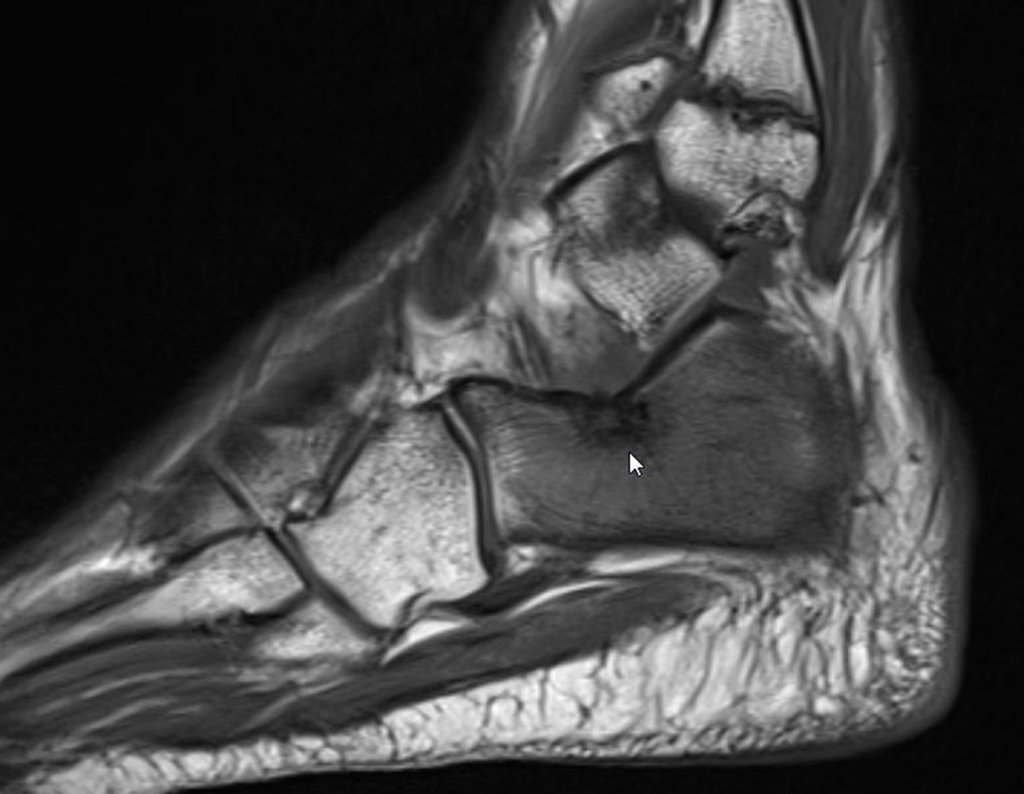
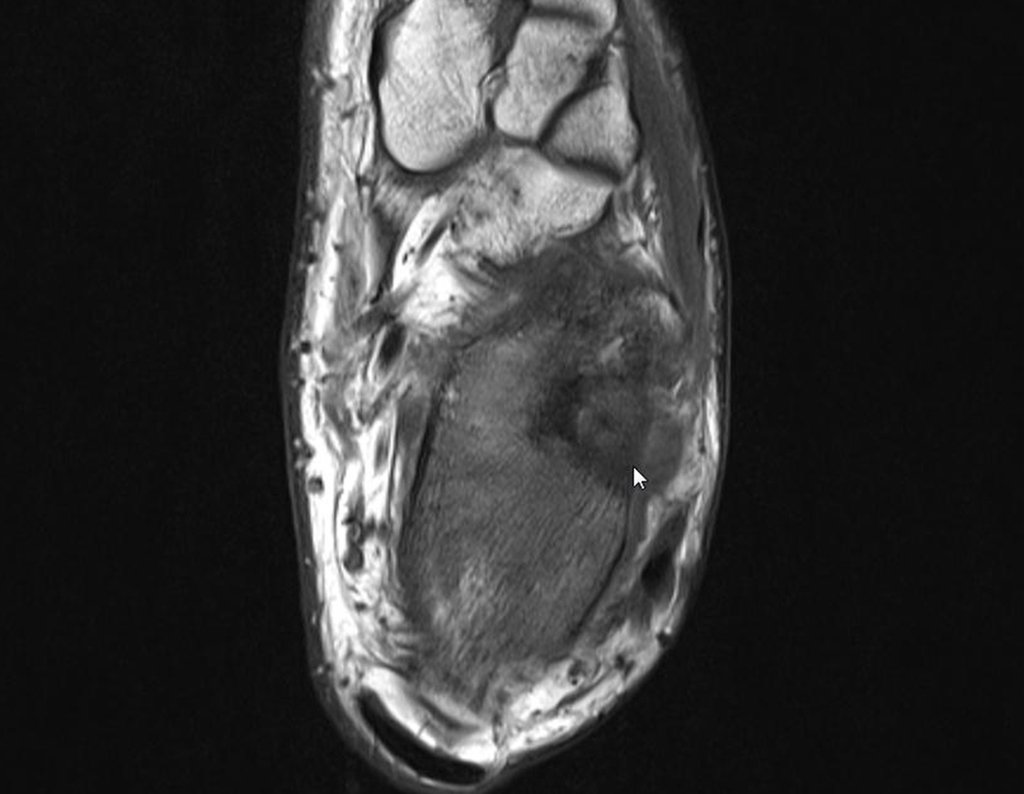
To better study the lesion, a bone tomography examination was performed, figures 9 to 14.
With the diagnostic hypothesis of osteoid osteoma, the orthopedist who accompanied him recommended treatment with radiotherapy. In April 2014, he underwent radioablation. During the first three months he used painkillers intermittently.
Four months after radioablation, due to the persistence of the painful condition, he underwent a new tomography on 08/17/2014.
The images from this computed tomography, after radioablation, are analyzed in figures 15 to 20.
What is the meaning of this image? Scar? Persistence of the injury? Does the patient still have the same symptoms?
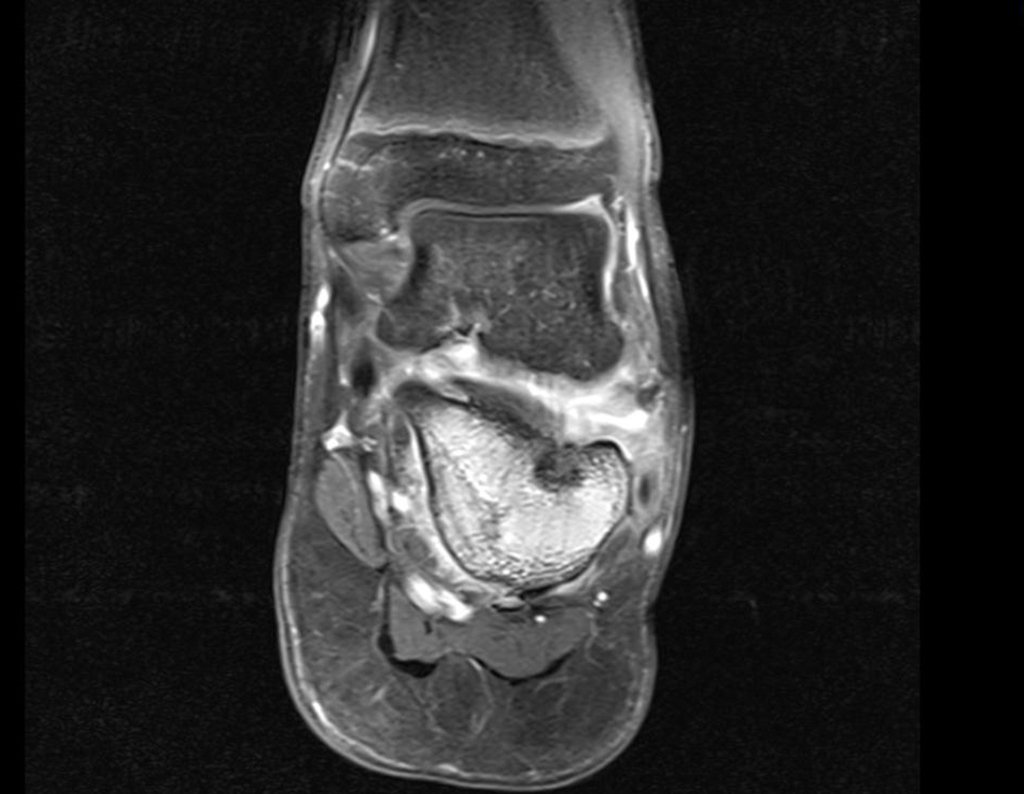
Analgesic physiotherapy and medication change indicated. Without improvement in symptoms, an MRI was performed to better assess the condition.
The patient is referred for a second opinion, being evaluated in December 2014, figures 35 to 39.
After careful analysis of the case and with unsatisfactory progress, the patient underwent surgery in January 2015, to resect the lesion and place an autologous iliac graft.
The removal of an iliac graft must also be performed with surgical access and adequate hemostasis. To do this, it is necessary to incise the skin above the iliac crest, only the skin and subcutaneous tissue, perform careful hemostasis with electrocautery and retract the skin distally, bypassing the insertion of the abdominal oblique muscle. This must be removed from the ridge, as if we were “ roaring ” the bone with an electric scalpel. You should not cut the muscle , as beginner surgeons usually do, as there will be bleeding.
This way we can achieve broad, safe access without unnecessary blood loss, figures 51 to 58.
Video 1: Preparing the graft.
The calcaneus is a load-bearing bone, and its reconstruction with autologous bone graft has the best integration, allowing early recovery of the patient’s function.
Return to the office 8 days after surgery.
Video 2: Six weeks post-operative, on 02/25/2015.
Video 3: Normal ankle mobility.
Video 4: Patient walking with full load – three months post-operative.
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com