Total Humerus Prosthesis in Osteosarcoma - Elbow and Shoulder Arthroplasty - Glenoid Capsuloplasty
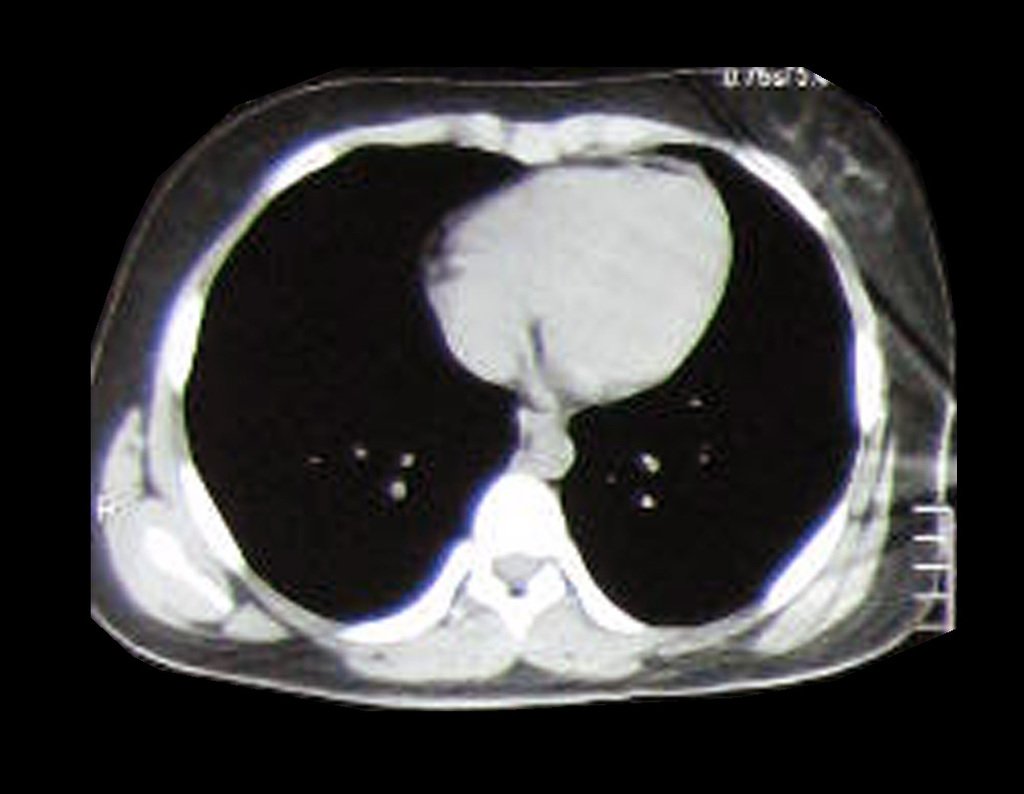
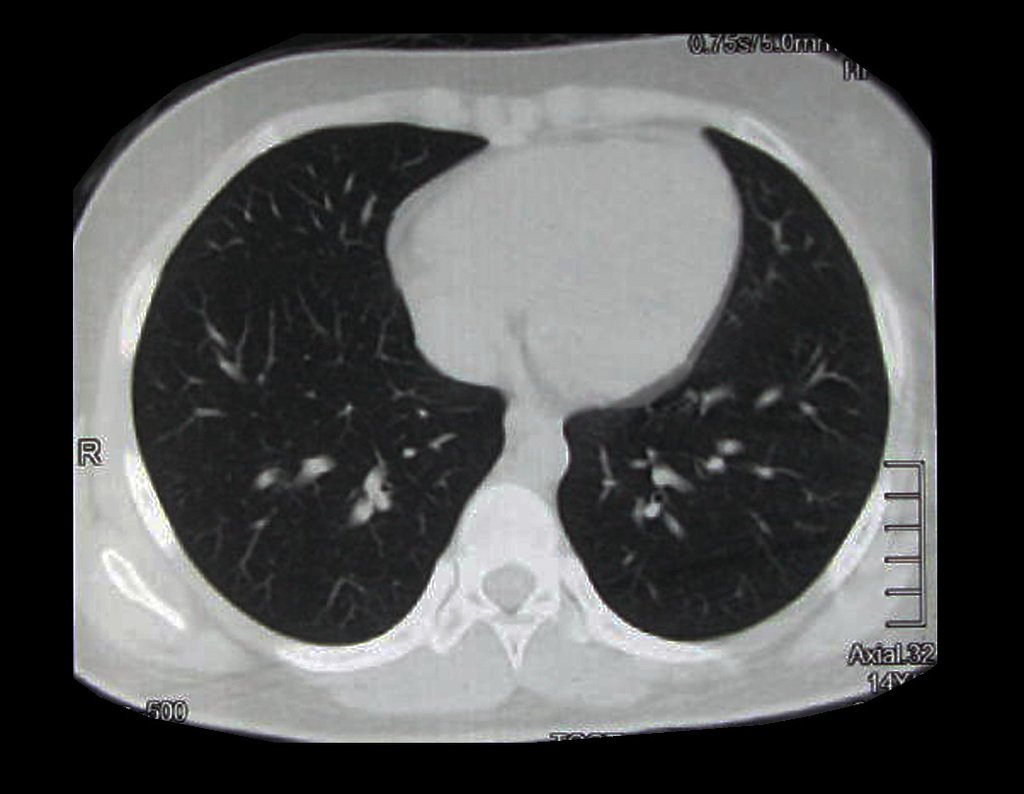
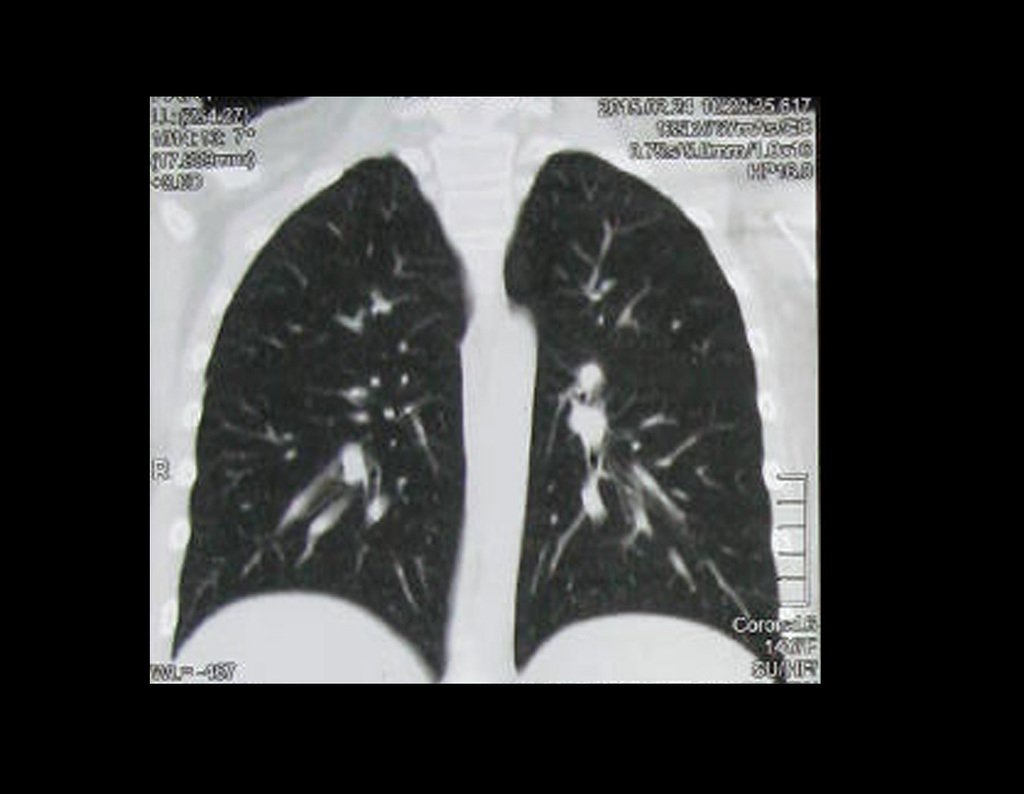
Total Humerus Prosthesis. Total Humerus Prosthesis Technique in Osteosarcoma. A 57-year-old male patient reported the appearance of low back pain at the end of October 2014, radiating to the MIE. Due to the progression of symptoms, he underwent a spinal resonance which reported the presence of a herniated L5-S1 disc. He started physiotherapy and with the worsening of symptoms he underwent a tomography on 02/18/2015, with reports of facet arthrosis L2-L3, L3-L4 and L5-S1 discopathy with protrusion into the medullary canal and x-rays of the pelvis, figures 1 and 2 .
The clinical appearance and function of the left upper limb can be seen in figures 27 to 29.
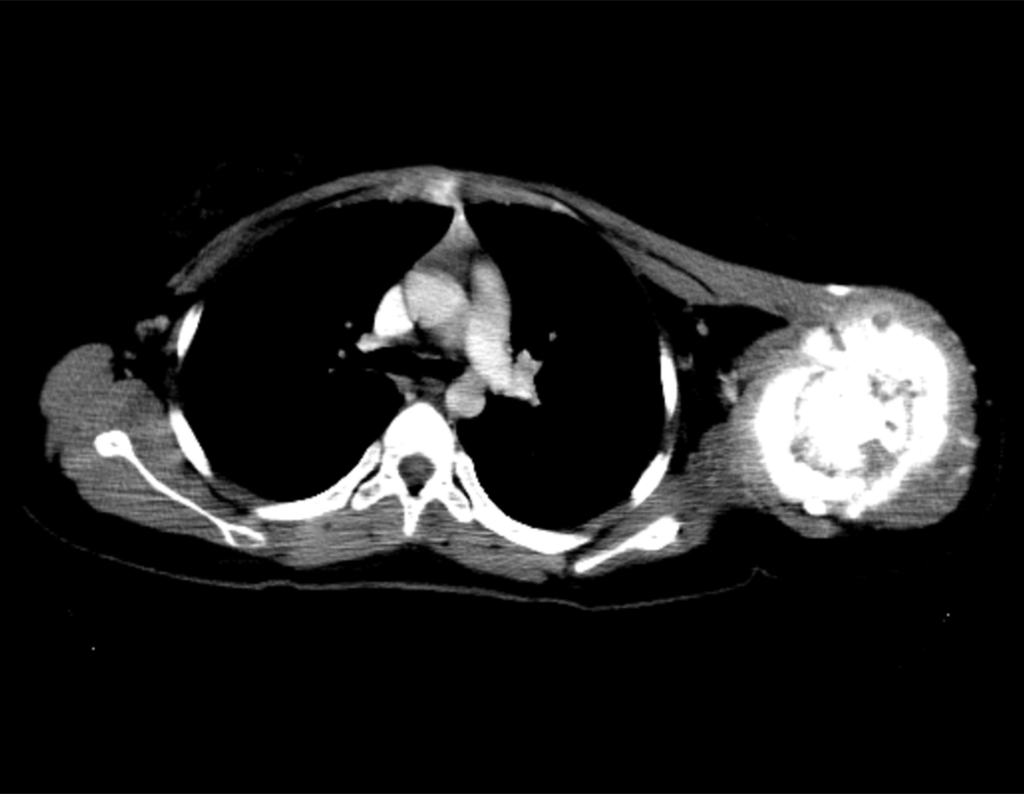
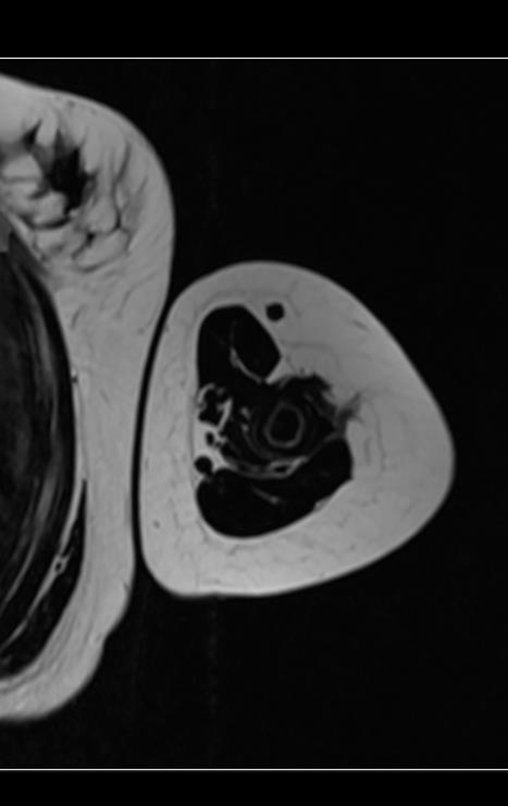
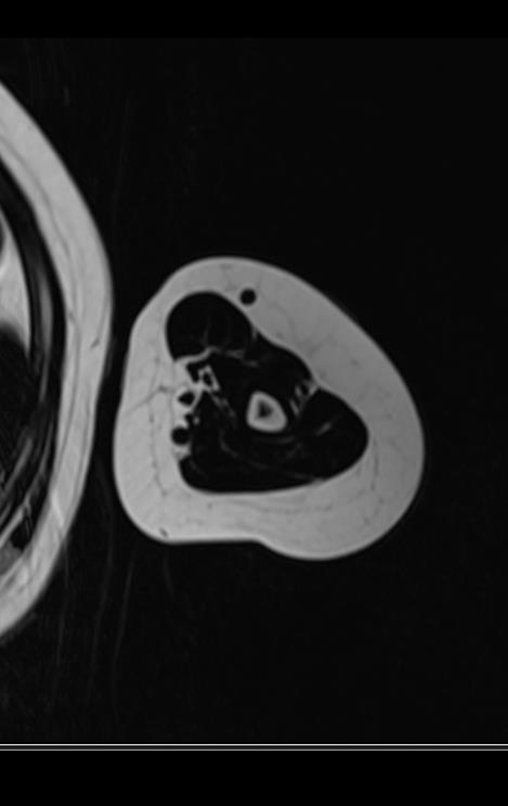
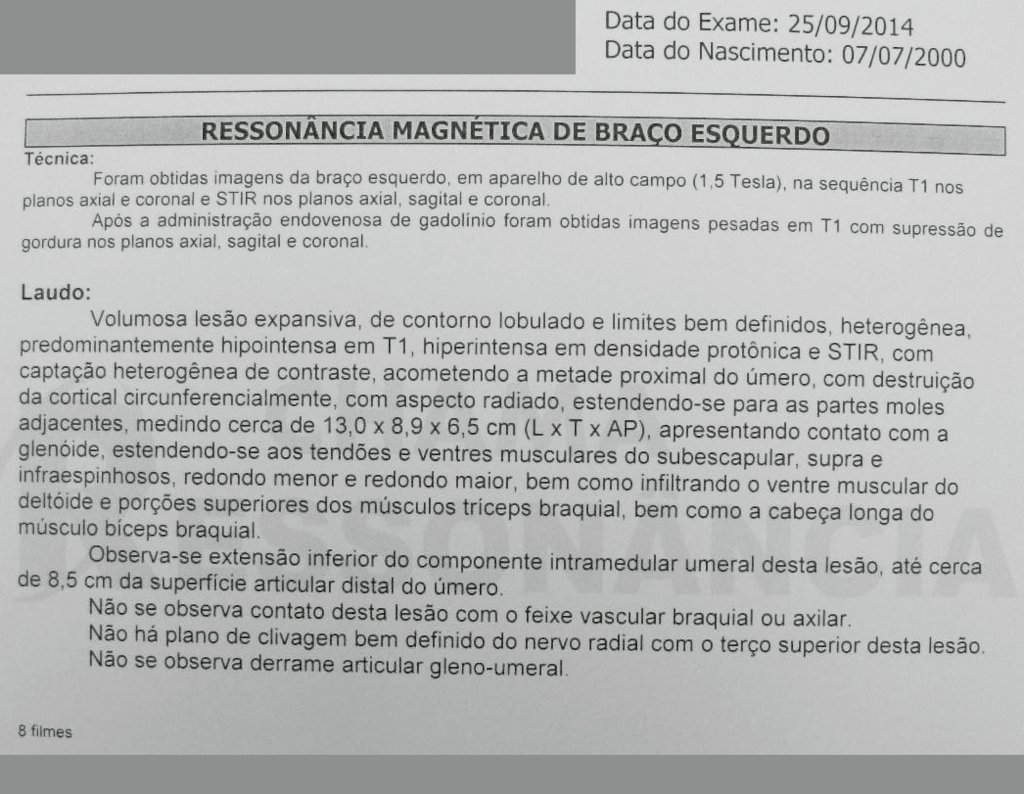
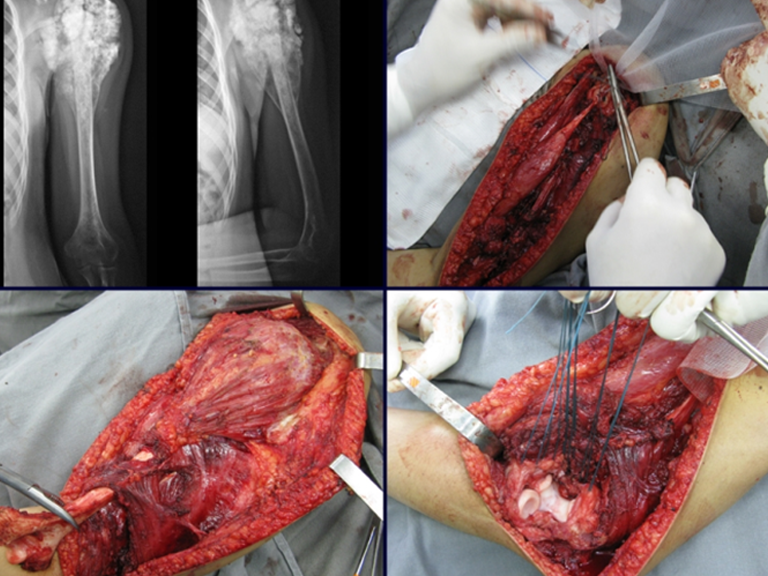
The study of the images and the analysis of the clinical examination showed the involvement of the deltoid muscle, but with the feasibility of conservative surgery, with margin, as long as the involved muscle was completely resected and the humerus was completely replaced with a modular polyethylene endoprosthesis.
Despite the need for partial functional sacrifice of the shoulder, and the need for arthroplastic reconstruction, with Marlex mesh for proximal coverage of the prosthesis and stability of the shoulder, preservation of the upper limb was our indication, aiming to offer a remaining cosmetic and functional aspect of the shoulder. satisfactory member.
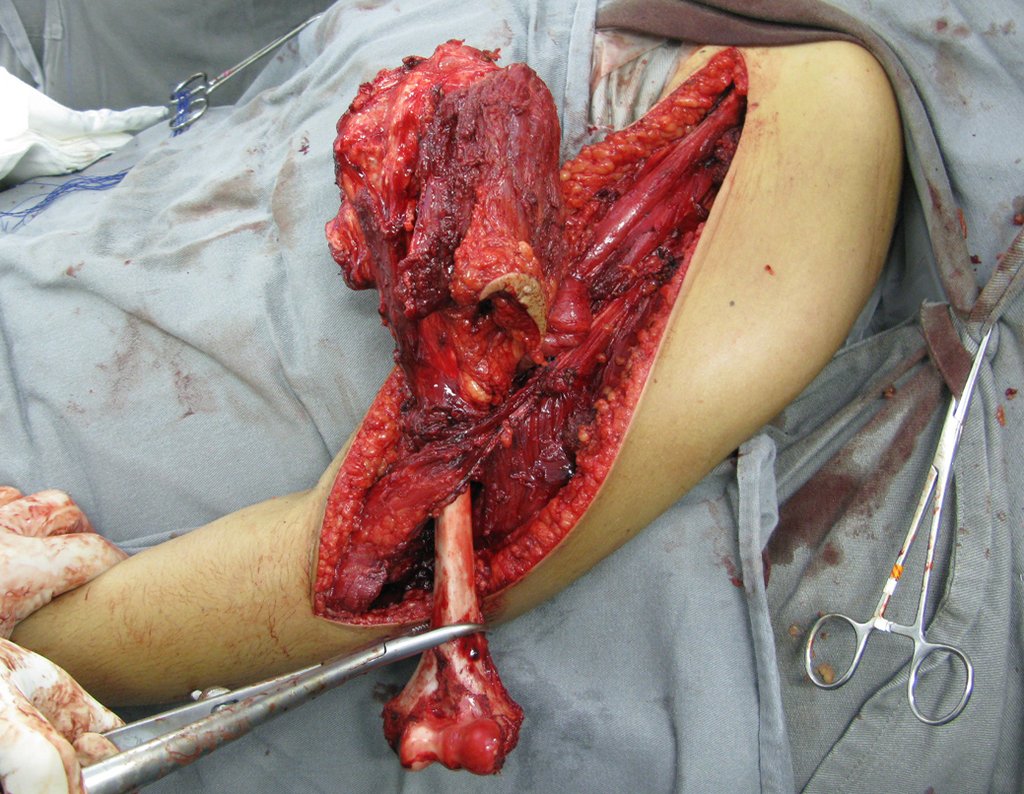
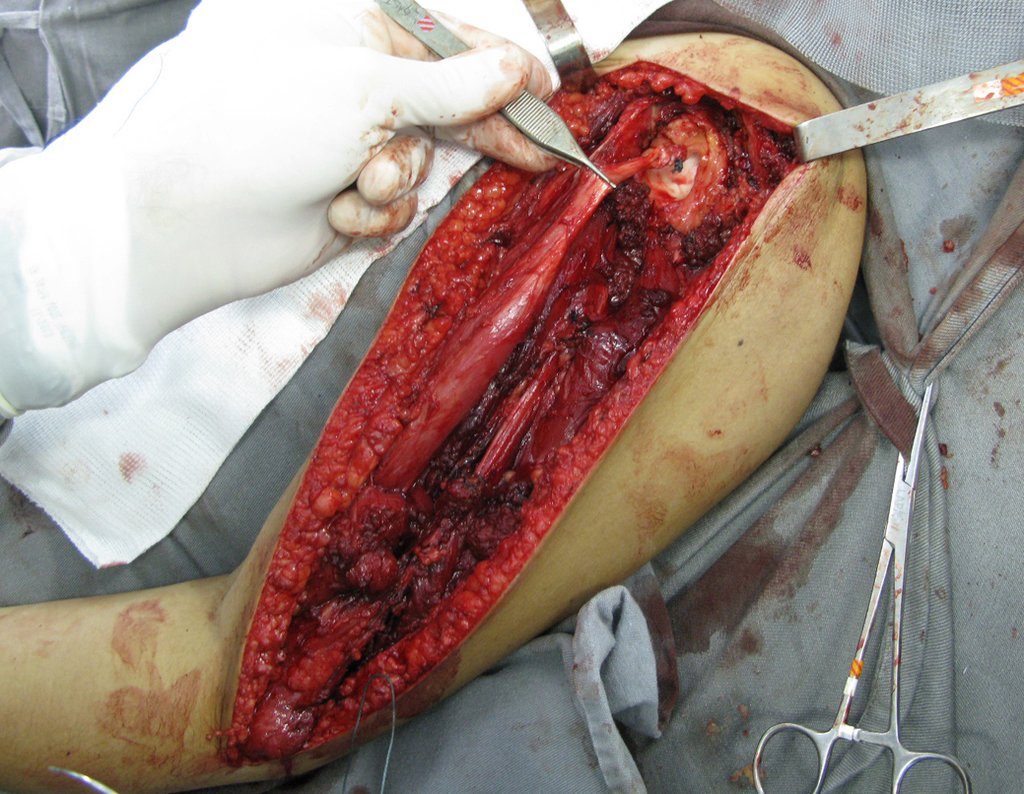
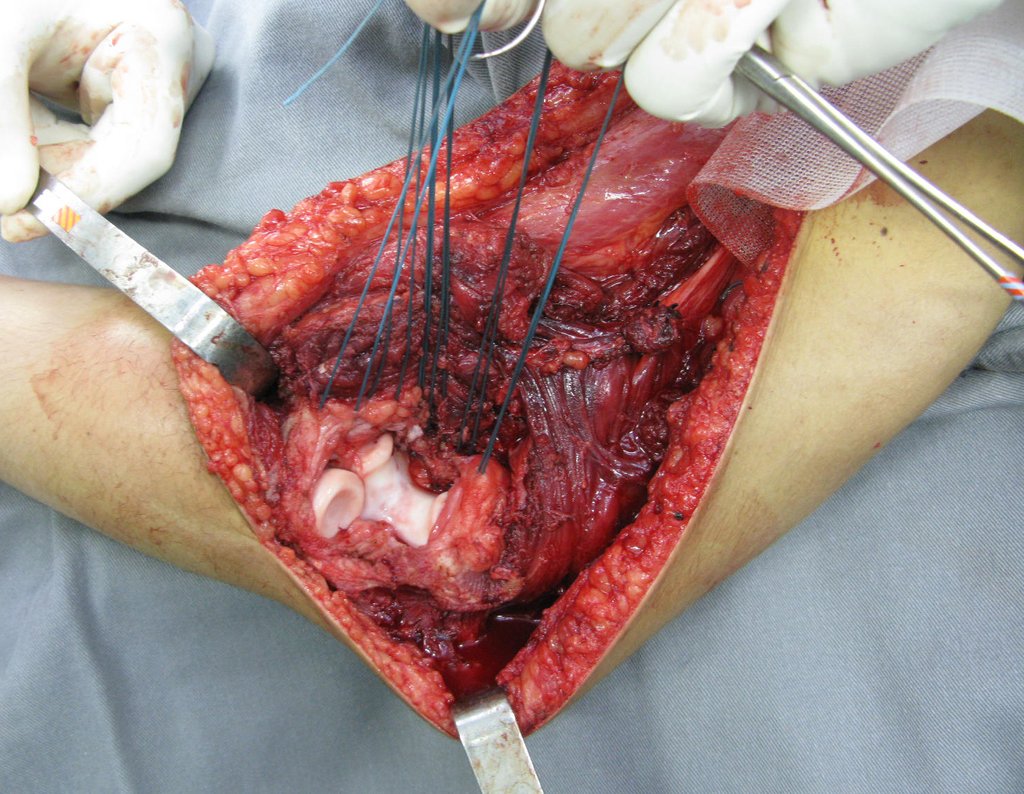
Total resection surgery of the left humerus, including the entire deltoid muscle, and reconstruction with endoprosthesis and Marlex mesh can be studied in figures 31 to 75.

Video 1 demonstrates the reinsertion of the long cable of the biceps brachii muscle.
Video 1: Marlex mesh suture around the glenoid.
As we could see, the entire deltoid muscle and biopsy tract, along with the joint capsule, were resected. Only skin and subcutaneous cellular tissue remained for the proximal coverage of the humeral reconstruction.
It is necessary to create a containment around the glenoid to stabilize the prosthesis, preventing its displacement. This containment mechanism needs to allow rotational movements of the humerus to provide adequate function.
To obtain this result we will describe our technique in detail. Video 2 illustrates the suture of a Marlex mesh around the glenoid, aiming to create a fixation point for the proximal portion of the humeral prosthesis that we used in this reconstruction.
Video 2: Fixation of the Marlex mesh on the anterior portion of the glenoid.
Video 3: Cementation and assembly of the proximal humerus prosthesis, defining at this point 20 degrees of internal rotation. There is a distal vent for excess cement to escape.
The polyethylene prosthesis is more suitable because of its lightness compared to a fully metal one. Polyethylene has an elasticity similar to that of bone and allows us to create holes at strategic points for the reinsertion of tendons and ligaments, which may have been shortened due to the need for a surgical margin during resection.
Video 4: We demonstrated good fixation of the wires and Marlex mesh in the proximal region of the total humeral prosthesis. This suture is performed with a pleat similar to a Scottish skirt, to allow rotational movements.
Video 5: Patient one week post-operative, good cosmetic appearance, starting physiotherapy.
Video 6: Wrist function 15 days after surgery. For now, only perform hand and wrist movements.
Video 7: Function in August 2015, nine months after total resection of the left humerus, with excision of the entire deltoid and reconstruction with total humeral endoprosthesis using Marlex mesh, to stabilize the prosthetic gleno joint. Good elbow flexion, excellent hand function and pronosupination and good humeral rotation.
Video 8: Patient in physiotherapy, flexing the shoulder with the help of the contralateral limb, on 09/09/2015
Video 9: Shoulder elevation with the help of the ball and support on the wall, on 09-09-2015
Authors of the case
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com