Osteosarcoma of the femur - Non-conventional knee prosthesis - Length discrepancy - Epiphysiodesis of the femur and tibia.

It is not enough to simply say that we should perform the biopsy on the “side” of the surgical incision. It is necessary to carefully plan what we call the SURGICAL INCISION PATH.
We should not cross the vastus lateralis muscle but rather look for the direction of the posterior intercept of the fascia that covers the vastus laterally.
This way we will have a resection that will preserve the entire muscle, aiming for an anatomical resection of the biopsy site. In addition, we will be helping to restore better functionality.
Pay close attention to the patient’s positioning to best execute what was planned.


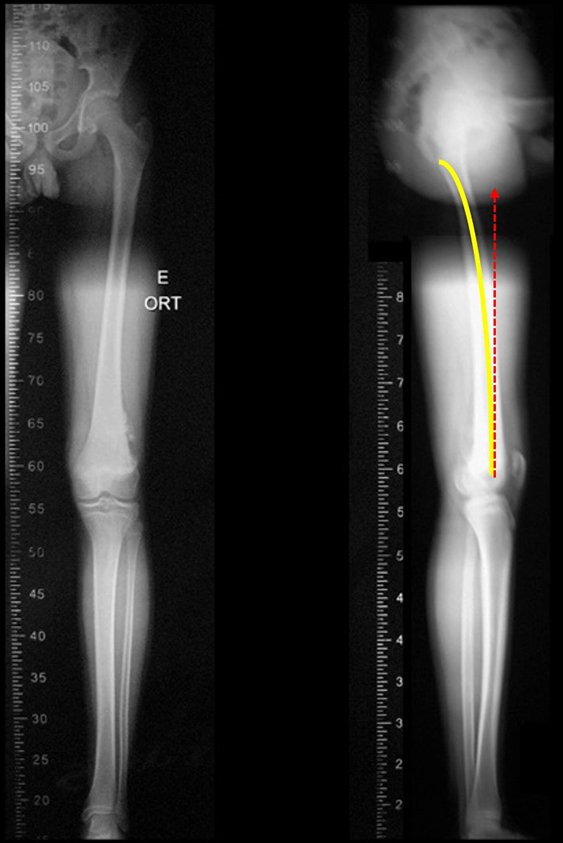
Scanometry in profile highlights the antecurvatum, marked in yellow, and the false path that the straight stem of the prosthesis would take, making it necessary to plan the special length of the stem and its thickness.
The model available in October 2015 had a round connection between the modules. Over time, they may loosen and rotate between them. The new modules requested feature rectangular blocks in the connections, yellow arrows A and B , in figure 29, in addition to the fixing screws being now stronger, white arrow. The new body of the prosthesis also features the rectangular fitting lock.
We requested ANVISA for authorization to manufacture a special model of this prosthesis, with the consent of the patient’s legal guardian, a minor, attesting to being aware that this model “Does not have the safety and efficacy evaluated by Anvisa”!!!
The prosthesis was made to order, with rectangular fittings between the modules and also in the fitting with the body of the prosthesis, blocking rotation. The rod was designed with the appropriate caliber for the patient’s spinal canal.
Note that the surgical field is dry, without bleeding. We detach the periosteum above the lesion limit and place a locked forceps to aid exposure.
Most of the dissection is carried out with an electric scalpel, from the subcutaneous layer, with low voltage, 20 cutting and 20 coagulation, in spray mode, calibrated to operate slowly, cauterizing slowly and avoiding burn injury.
We continue releasing the lesion, “”seeing” it with our fingers.
Video 2: Osteotomy with Gigle saw.
Video 3: Release of the cruciate ligaments.
We then prepare the tibial plateau to insert the tibial component of the prosthesis.
We only remove the cartilage from the tibia, removing the minimum amount of spongy bone tissue, which is firmer just below the cartilage. We regularize the tibial plateau, so that the surface is parallel to the ground, correcting the cut thickness, since the medial plateau is inferior to the lateral one.
This plateau osteotomy can be performed with a power saw or carefully with wide, sharp osteotomes.
Video 4: Regularization of the tibial plateau with osteotomes.
Video 5: After accommodation of the tibial component, the resection is checked and equalized with the size of the femoral prosthesis.
Video 6: Widening of the medullary canal, initially with a manual drill.
Then we complement it with motor milling.
Video 7: Complementing the widening with a motorized milling cutter.
Video 8: Channel widening depth test.
Video 9: Regularization of the top of the osteotomy.
Video 10: Compaction of the first prosthesis module.
Video 11: Compaction of the second prosthesis module and femoral stem.
Video 12: Fixing with four screws in each connection.
Once the components have been assembled and tested, we carry out the cementation, starting with the tibial component, reduce it and carry out the last text, before placing the femoral plug and final cementation.
Video 13: Cementation of the tibial component and removal of excess cement.
Video 14: Cementation of the femoral component.
Video 15: Testing the functional range of the knee with the prosthesis.
Video 16: Placement of soft tissue hemostat.
Video 17: Walking with the immobilizer, on 01/05/2016, twenty days after surgery. (third week), walking slowly.
Video 18: Walking with the immobilizer, third week, guiding posture.
Video 19: Macha with the help of the physiotherapist’s two hands, faster, automating.
Video 20: Walking with the immobilizer and assistance, slight knee flexion.
Video 21: Starting to walk with a crutch, on 01/05/2016, three weeks after surgery.
Video 22: Walking training, now with a long knee brace, removing the foot from the ground and slightly flexing the knee, on 01/06/2016, second day of assisted physiotherapy.
Video 23: Walking with the knee free, on 02/17/2016, two months after surgery. Slight flexion and lameness.
Video 24: March on 03/30/2016, after 3 months. Improvement of lameness.
Video 24: Patient sailing, balancing with his lower limbs, in July 2016, after eight months of surgery.
Video 25: Skiing, in July 2016, after eight months of surgery.
Video 26: March on 07/12/2016, after 8 months. Symmetrical function, without lameness.
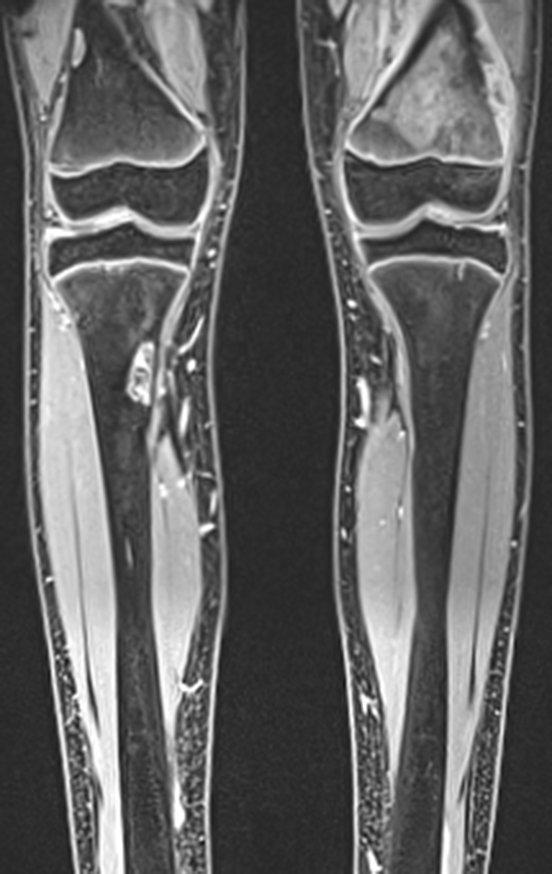
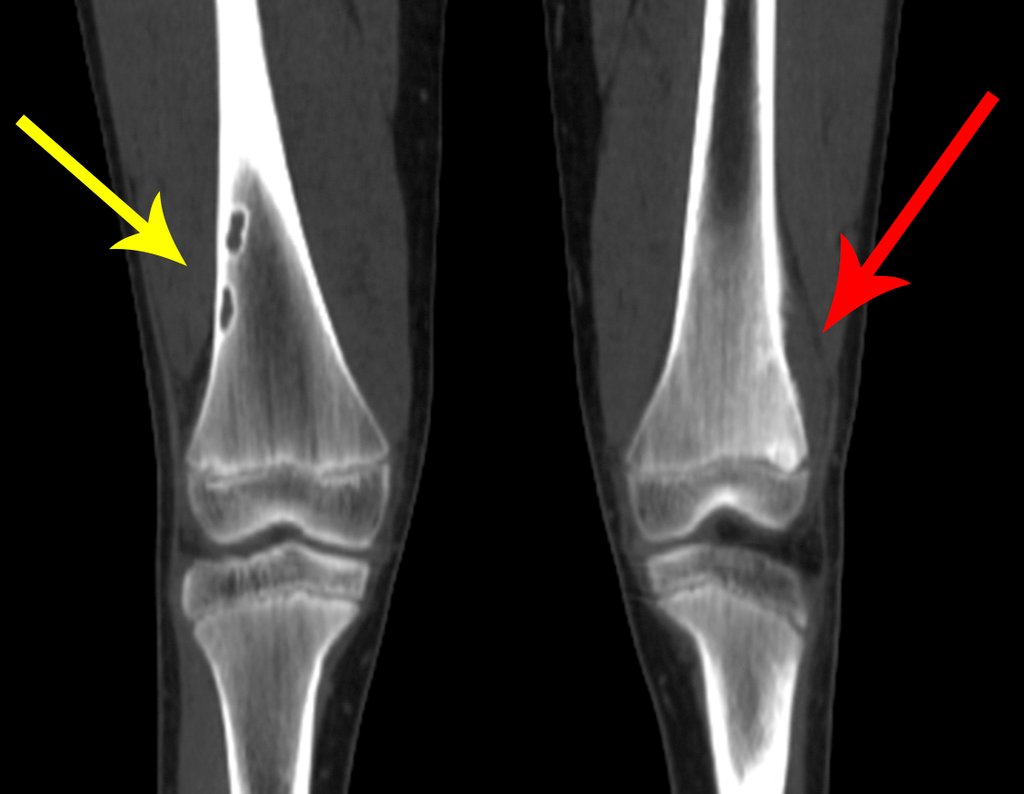
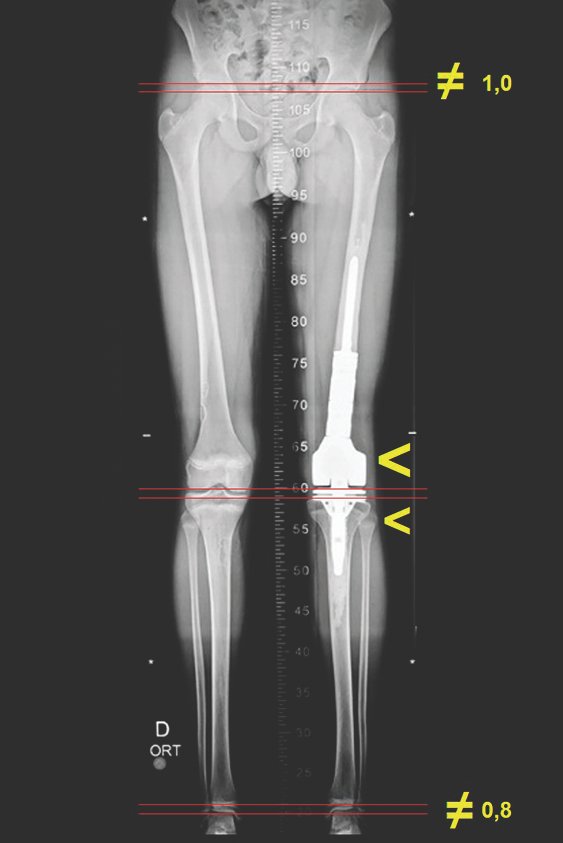
Although we left the operated limb longer, the patient had a significant growth spurt causing the length discrepancy. This stretch, however, corrected the flexion attitude of the operated knee. This metallic prosthesis causes a greater discrepancy in the length of the limbs because, in addition to the resection of the femoral plate, the tibial component greatly damages the growth plate, and blocks the remaining physis due to its cementation. With the patient off chemotherapy, we scheduled definitive epiphysiodesis of the growth plates of the femur and contralateral tibia, aiming to stabilize the discrepancy.
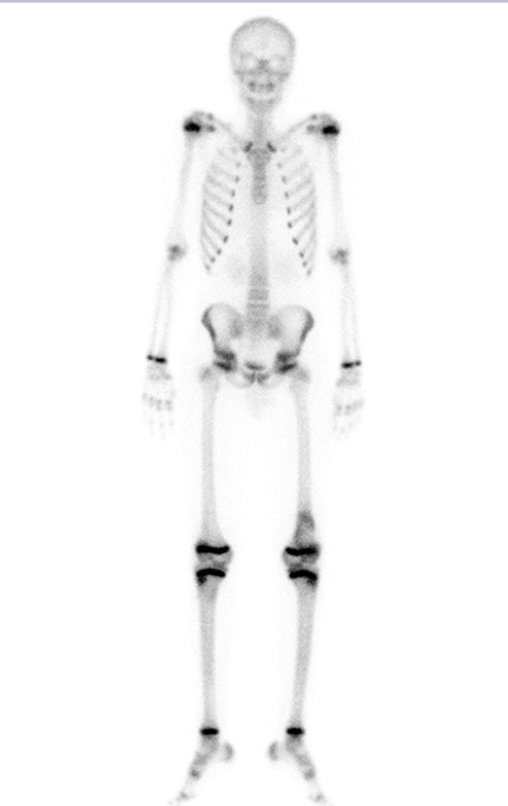
Realizada a epifisiodese do lado contralateral. Após três meses, podemos observar que o fechamento das fises já acontece, comparando as cintilografias pré, figura 81, e pós, figura 82.
Video 27: Symmetric function in March 2017.
Video 28: Symmetric ability and function.
Authors of the case
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com