Myxoid Liposarcoma
Myxoid liposarcoma. Male patient, 28 years old, reports pain and progressive bulging in the posterior region of the right thigh, distally, 08 months ago, denies local trauma. Initially he sought an orthopedic service, a biopsy was performed and myxoid liposarcoma was diagnosed.
Referred to our service, we found an extensive tumor on the posterior surface of the thigh, starting in the middle third to the joint line, without pain or neurological deficit.
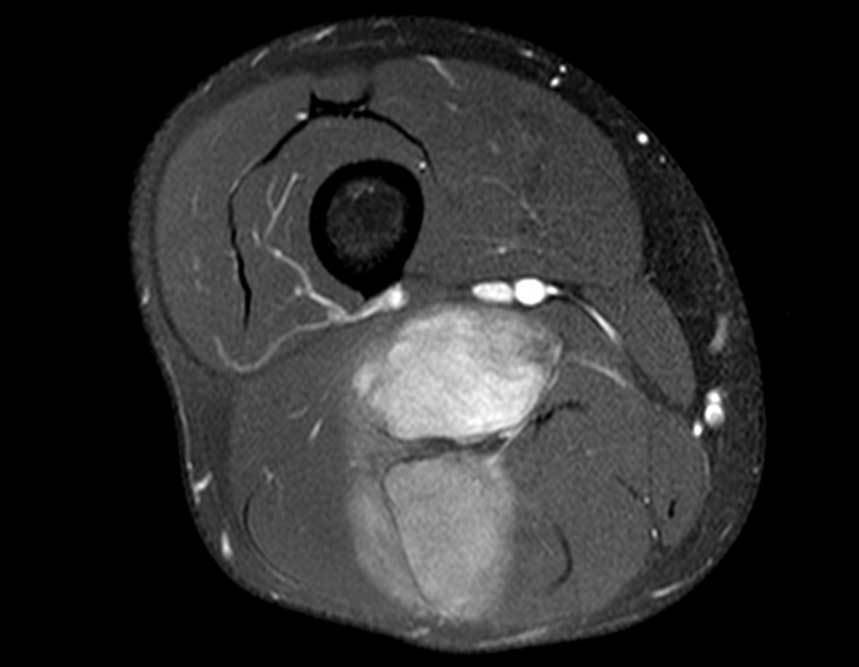
Magnetic resonance imaging, figures 1 to 14, demonstrate the heterogeneity of the lesion and its aggressiveness, showing the large extent of the lesion and its proximity to the vascular-nervous bundle.
After carrying out anamnesis, physical examination and complementary tests on the patient, we put forward some diagnostic hypotheses. As the patient underwent a biopsy at another service, we discussed the biopsy slide with the local pathology team who analyzed the material and after discussing, we arrived at the diagnosis of chondromyxoid liposarcoma.
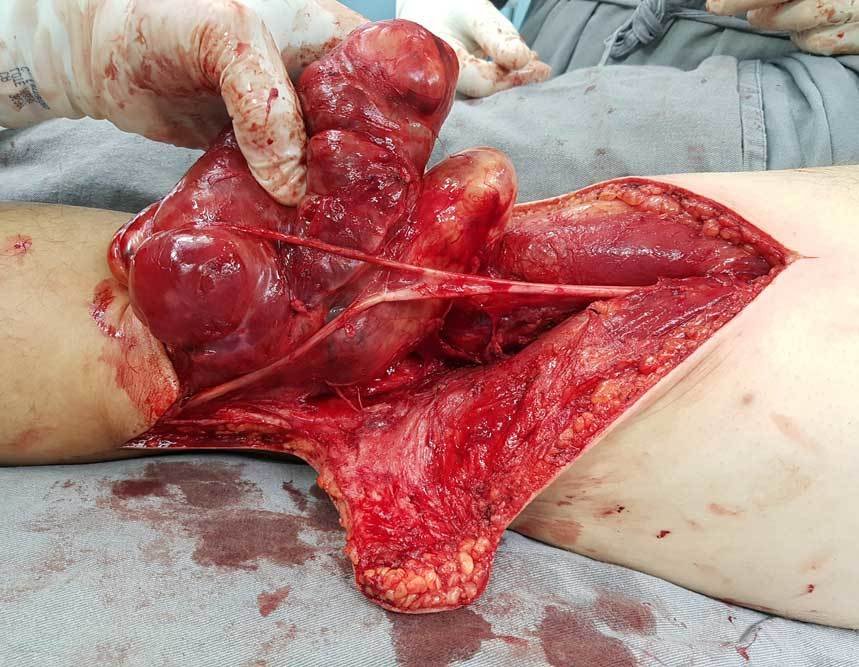
We talk to the patient about their pathology and treatment (resection + complementation with local radiotherapy at the discretion of the radiotherapist), we schedule the surgical resection with them accordingly. The following images explain the surgical step by step.
Patient in the post-operative segment, returns for consultation, without complaints at the moment, with good function of the operated limb and carrying out all his work activities as a Personal Trainer.
Case Author
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com