Giant Cell Tumor of the Tibia Intraepiphyseal Prosthesis
Giant cell tumor of the tibia. A patient born in April 1973, she presented with a bone rarefaction lesion in the right tibial epiphysis, when she was only fourteen years and six months old. In January 1988, she underwent surgery in Salvador – Ba and underwent curettage of the tumor. The anatomical pathological examination diagnosed it as a giant cell tumor, which is rare in the patient’s young age group.
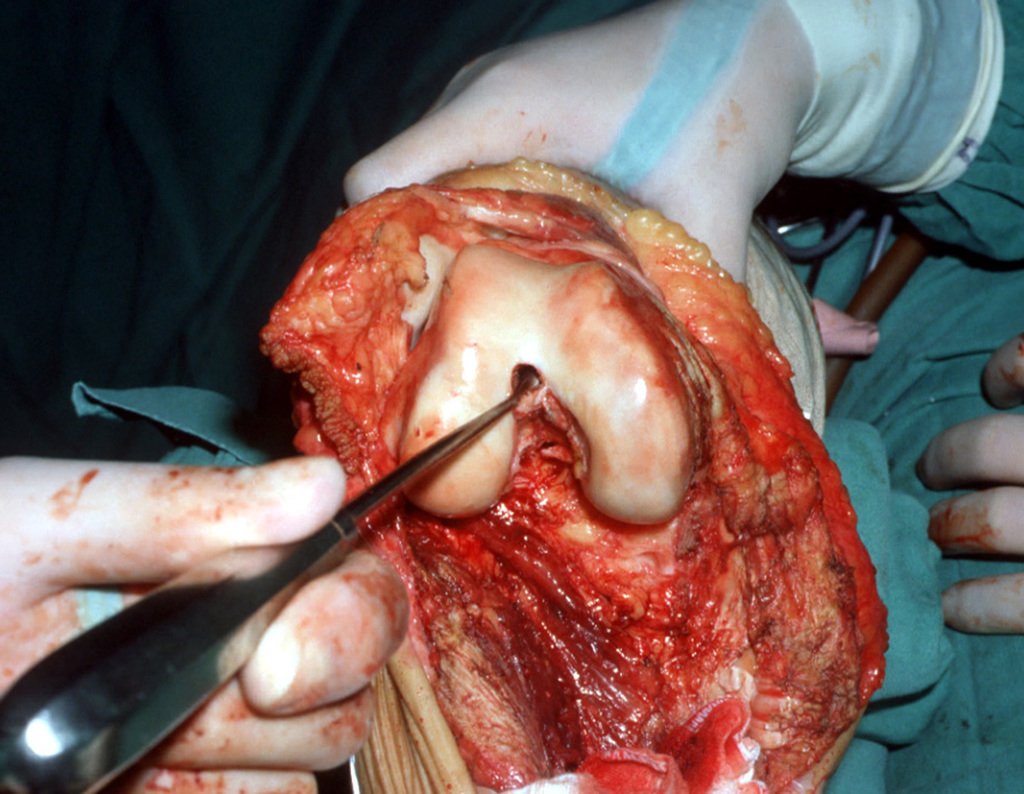
In February 1989, the patient underwent reoperation in the city of Vitória da Conquista, due to tumor recurrence. In June of the same year, she came to us due to a new recurrence, figures 1 to 3.
Despite the patient being very young, we opted for en bloc resection, due to two recurrences and tumor implantation in soft tissues. We designed a special prosthesis for this case, creating a model with an intra-epiphyseal component in the femur and replacement of the proximal third of the tibia, both components made of polyethylene.
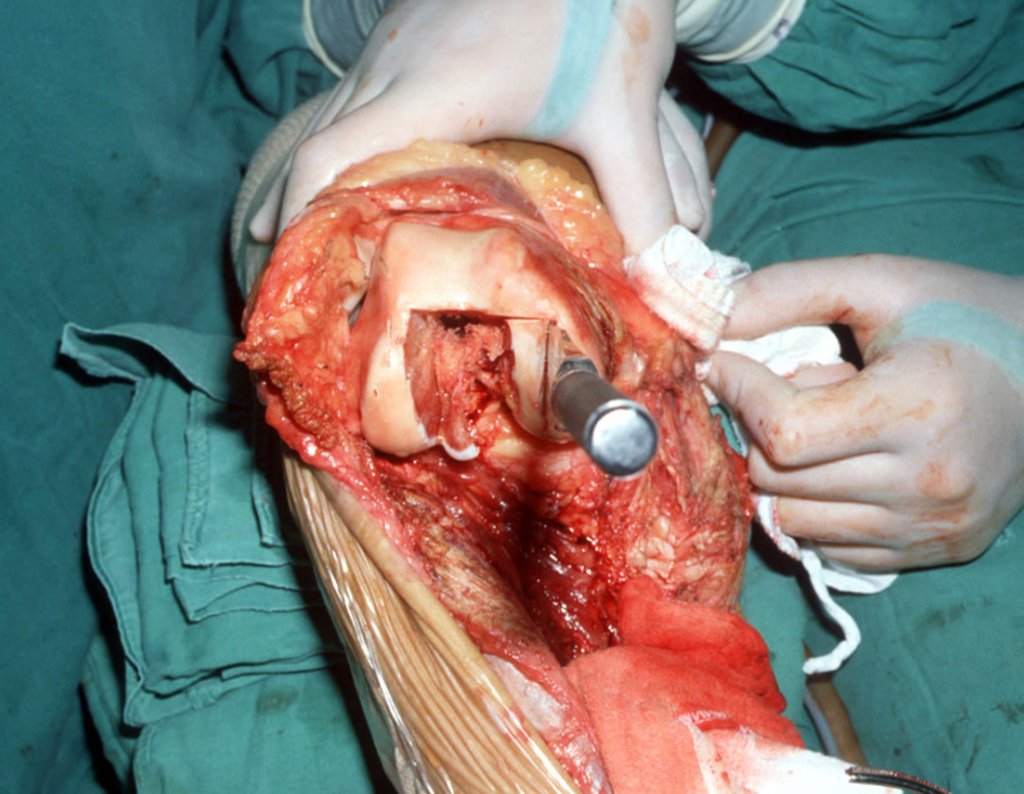
The resection was carried out en bloc, on 06/03/1989, with removal of the entire affected area, figures 4 to 15.
The reconstruction will be carried out with the prosthesis designed especially for this patient, made of polyethylene and stainless steel and with an intraepiphyseal component in the femur, figures 13 to 15.
The patellofemoral cartilage must be preserved as much as possible. Using the curette, we locate the femoral canal, figure 16. The femoral component will be fitted between the femoral condyles. To do this, it is necessary to perform a rectangular osteotomy, allowing adequate positioning of the component, figures 17 and 18.
This was the first intraepiphyseal prosthesis we performed. At that time, in 1989, we did not have cutting guides and the surgeon made the cuts by hand, using his skill to follow clinical parameters.
Patient residing in another state, dancing lambada, which was the rhythm of the time, figures 33 and 34. In January 2007, he sent this photo for our evaluation, figure 35. In February 2008, he suffered a fall resulting in a fracture of the femur, just above the femoral component, which was treated closedly, figure 36.
The fracture had malunion, with shortening and rotational deviation, resulting in protrusion of the femoral component, leading to functional limitation of the knee, requiring revision, figures 37 and 38. In 2009, the endoprosthesis was revised, figures 39 and 40 .
Authors of the case
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com