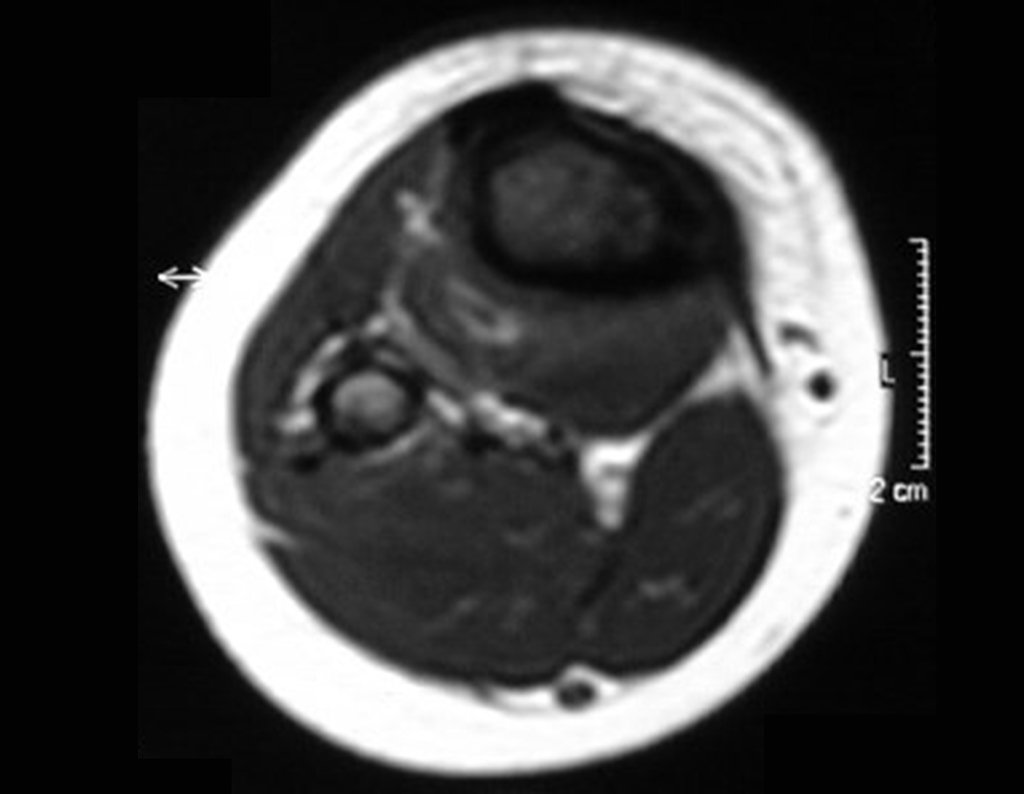
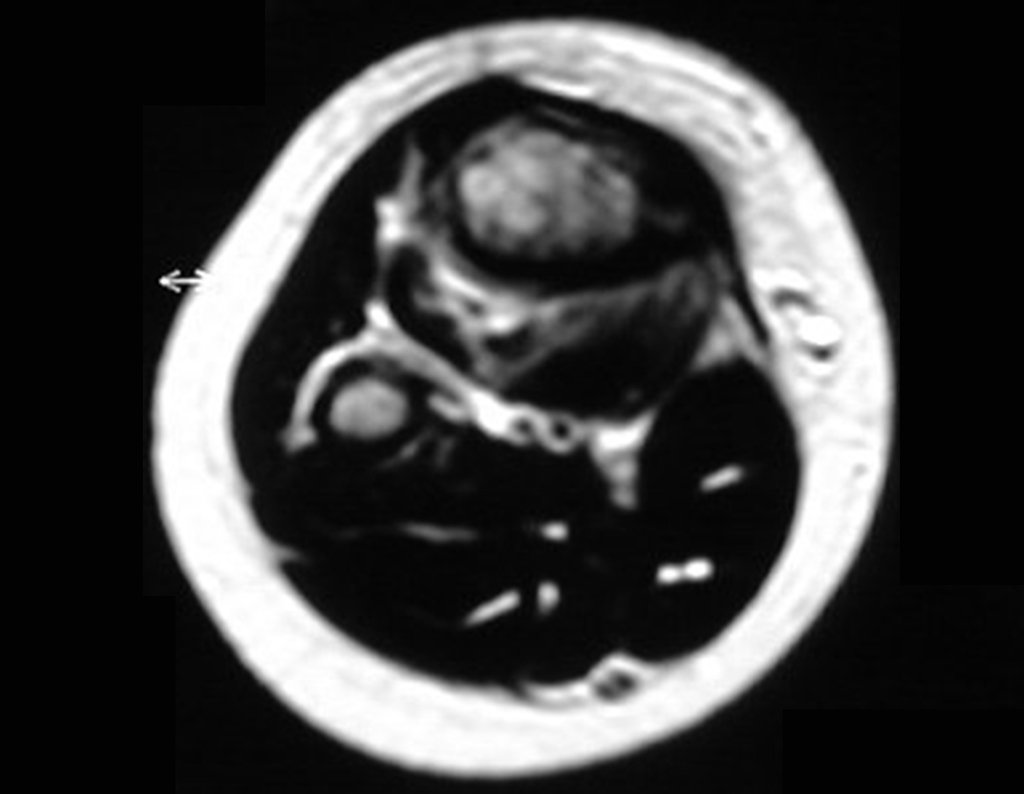
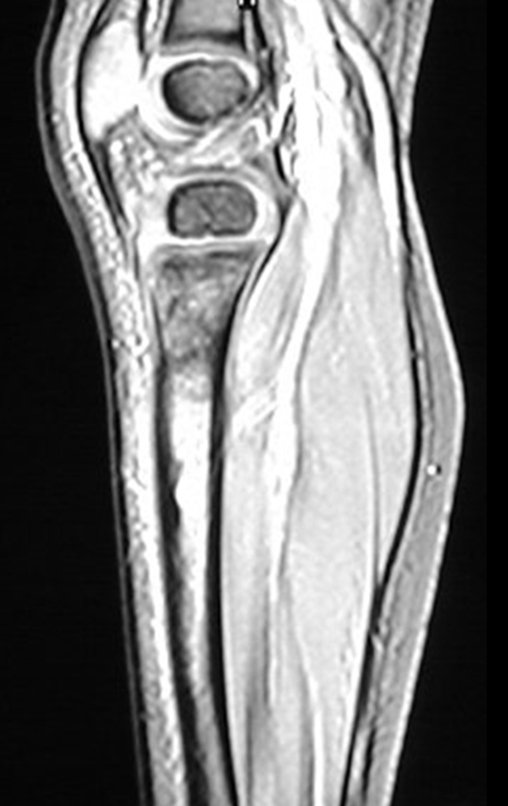
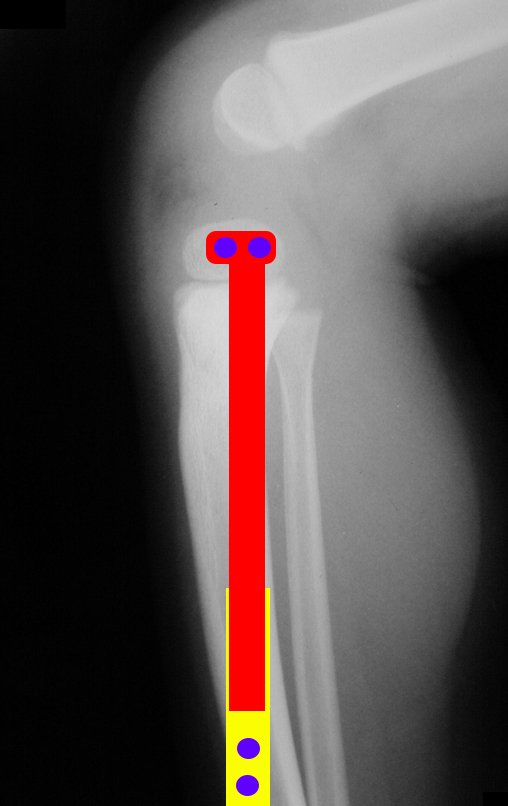
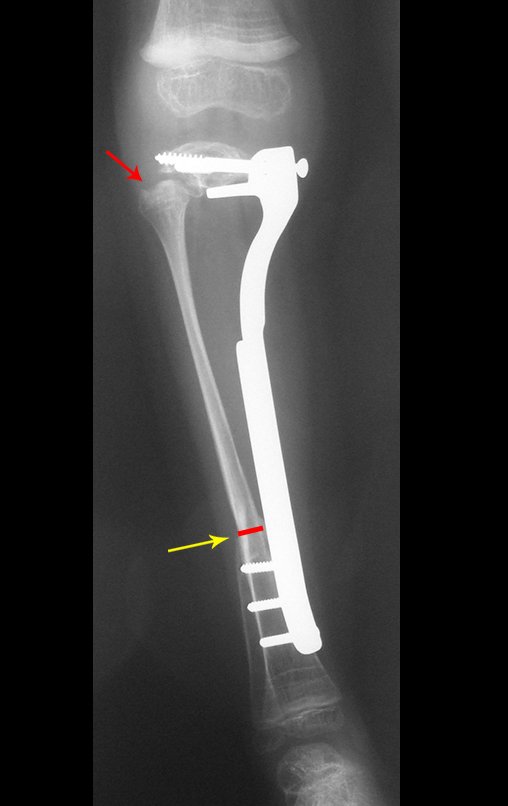
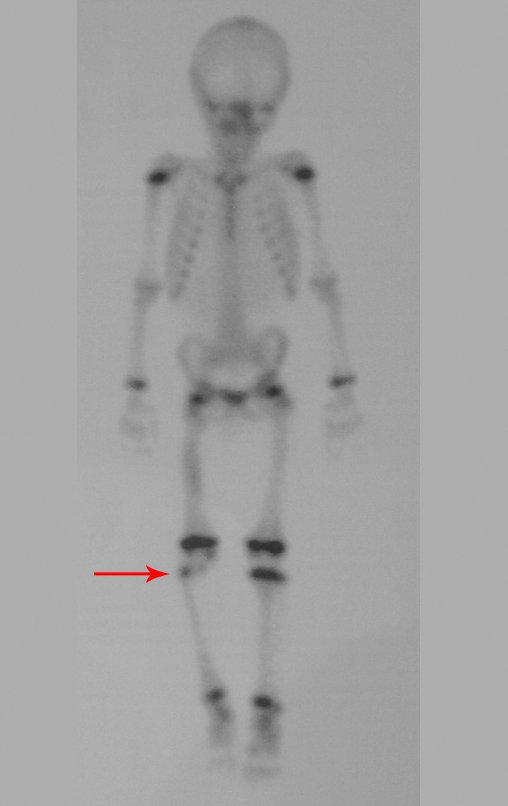
Ewing sarcoma of the tibia
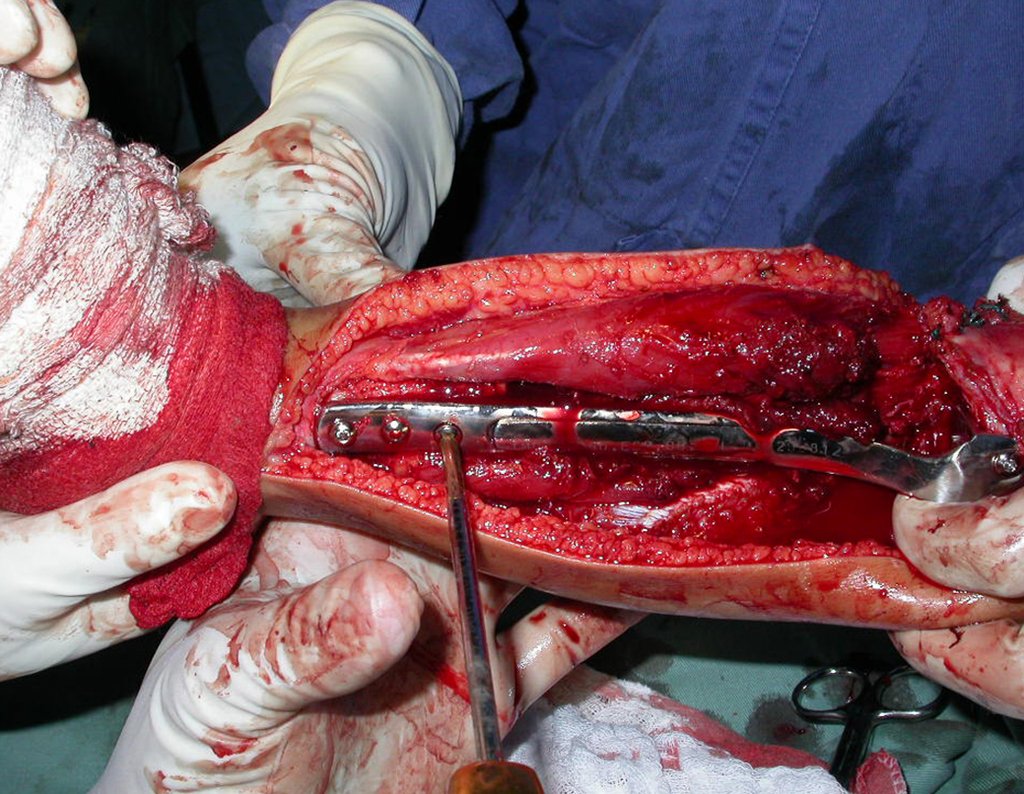
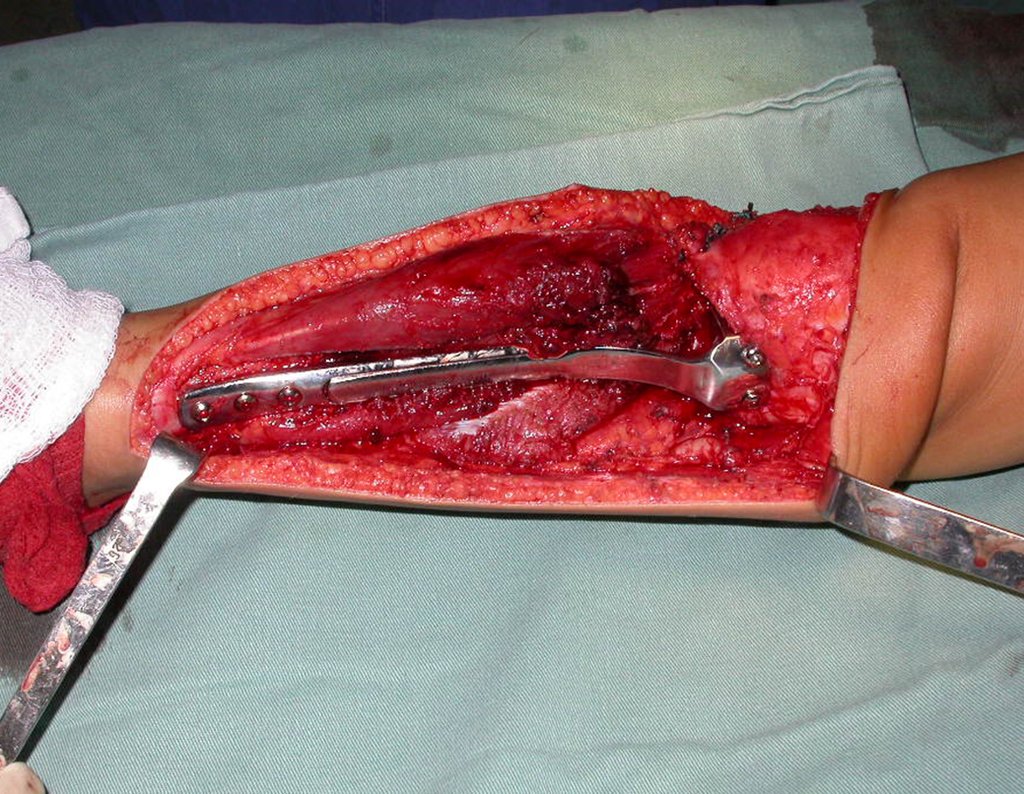
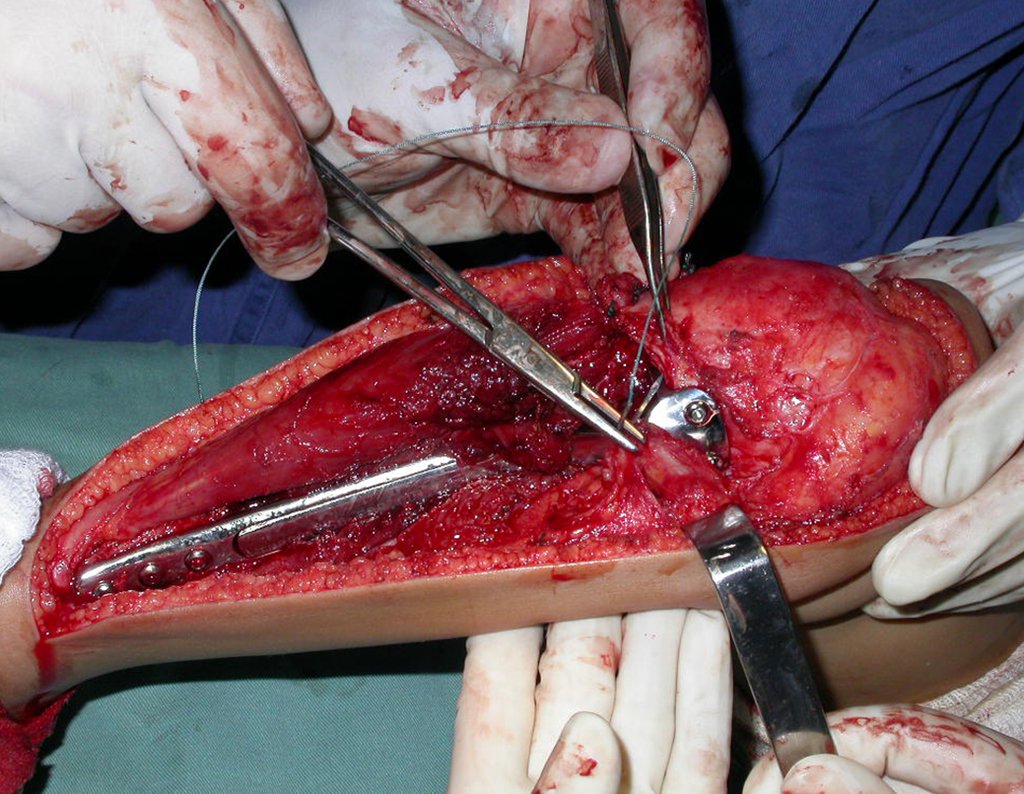
Video 1 : Demonstration of the sliding plate mechanism, which runs in a trapezoidal fitting similar to that of a lathe.
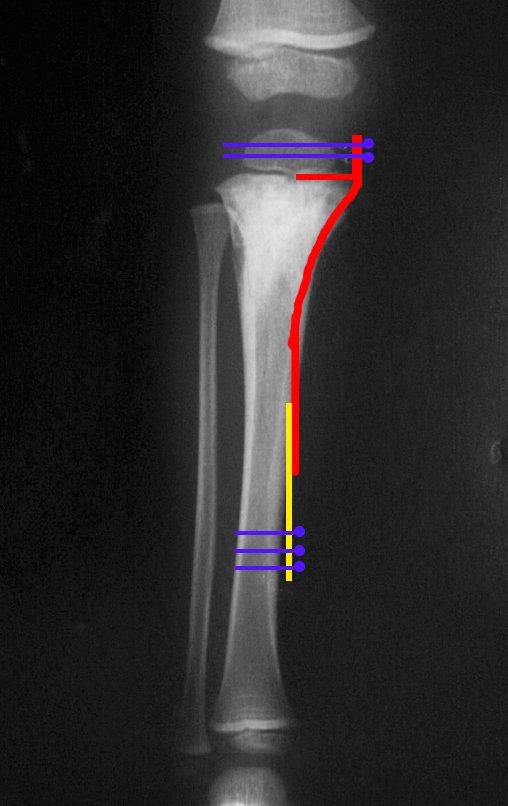
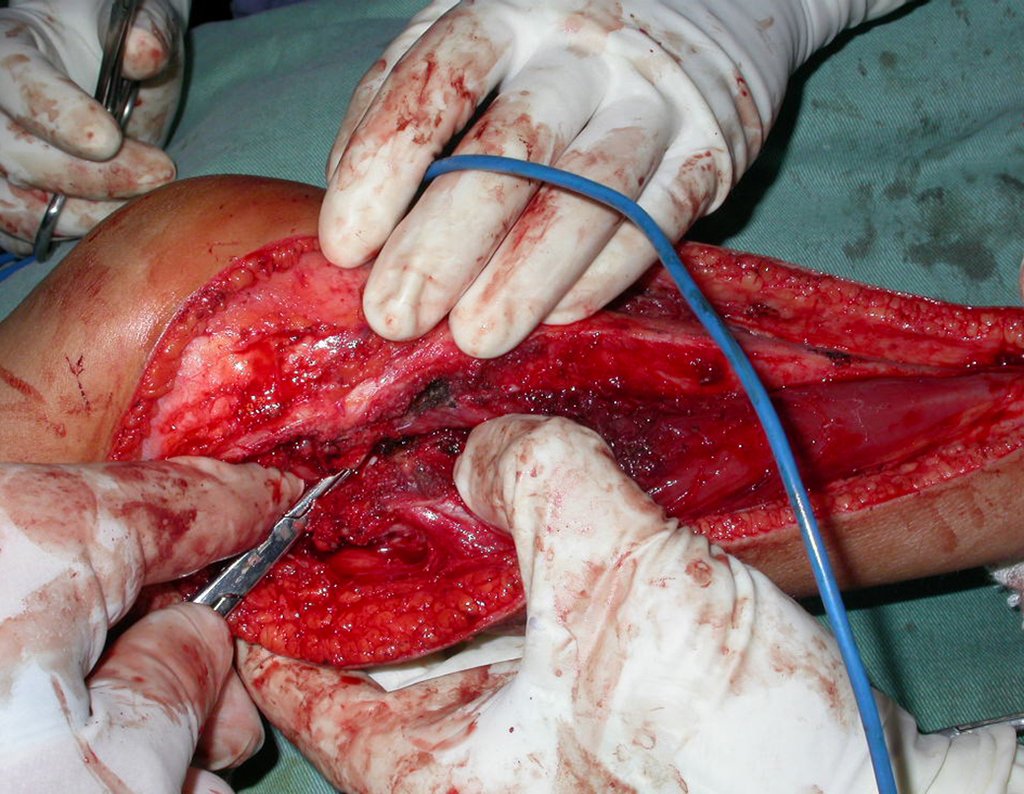
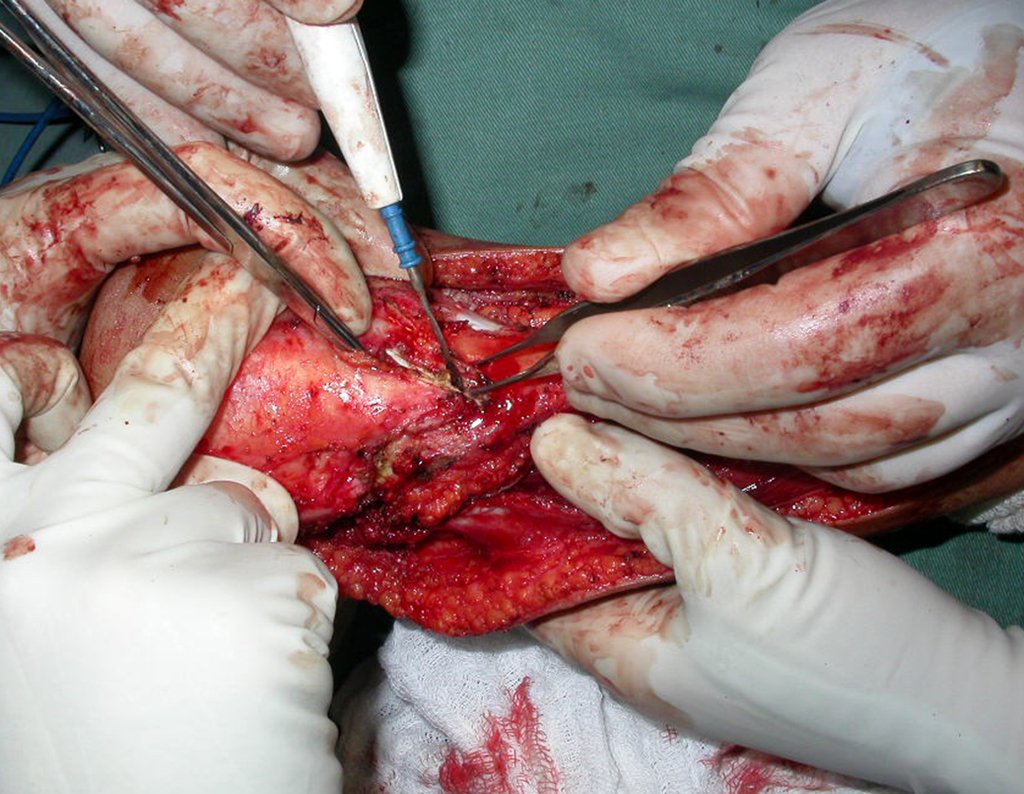
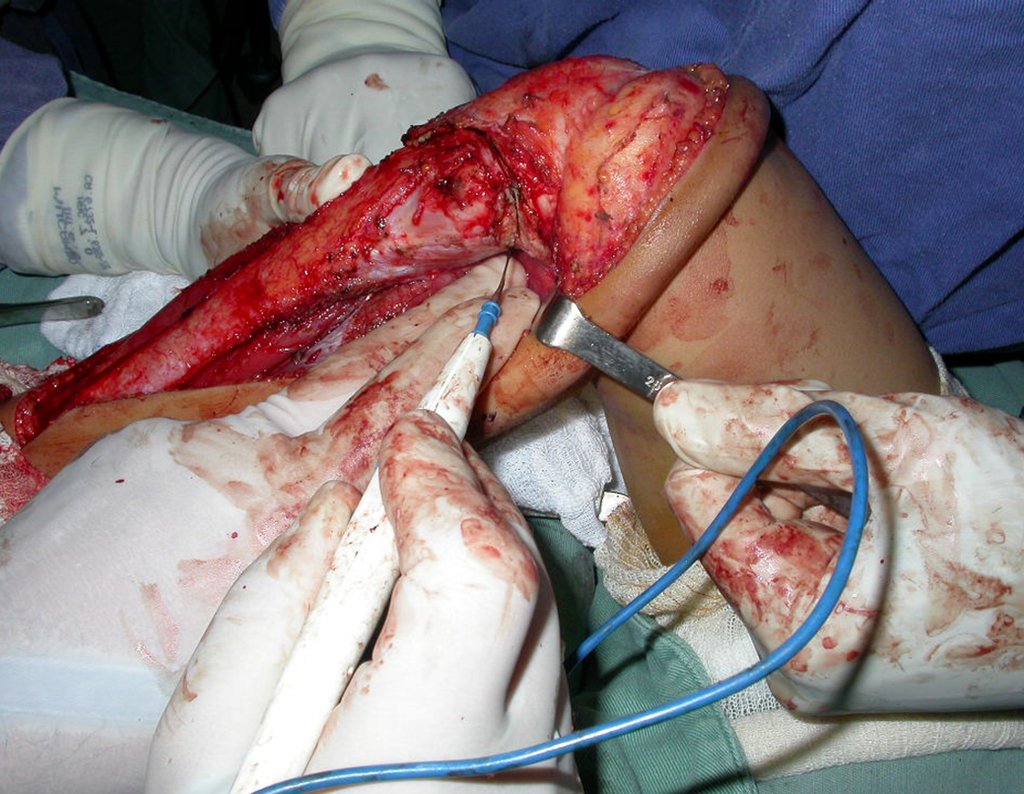
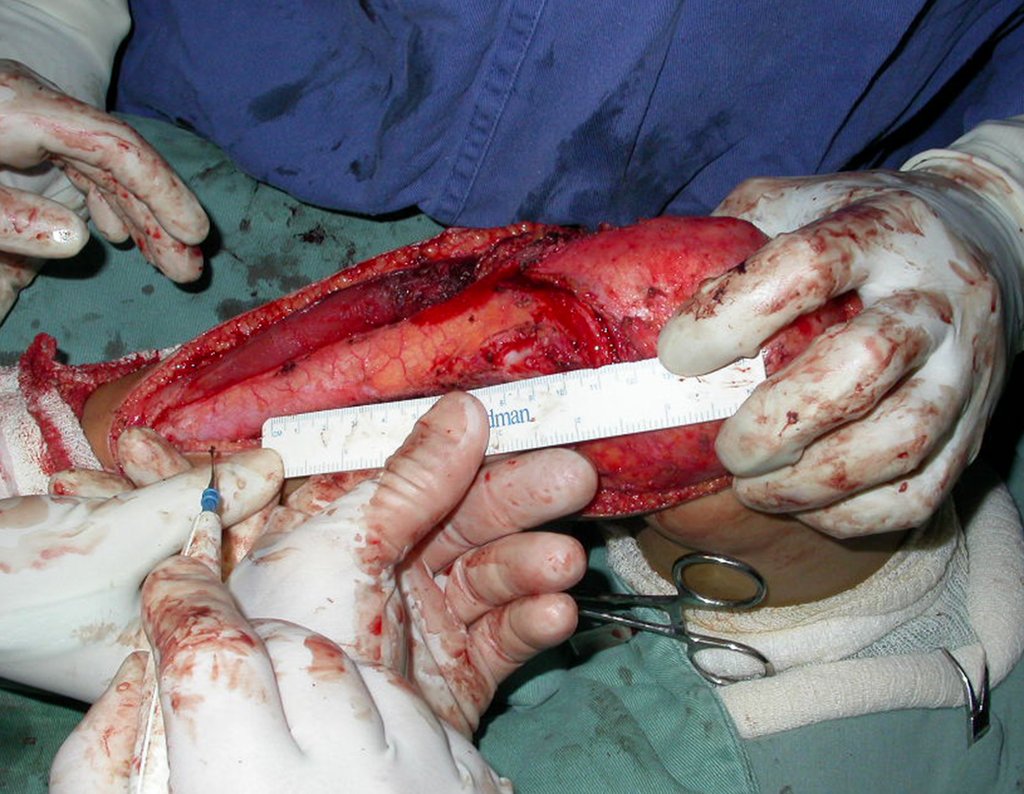
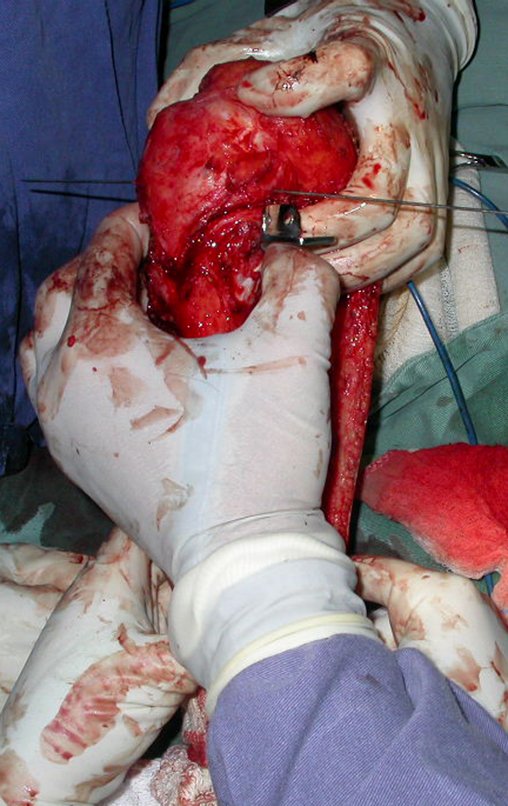
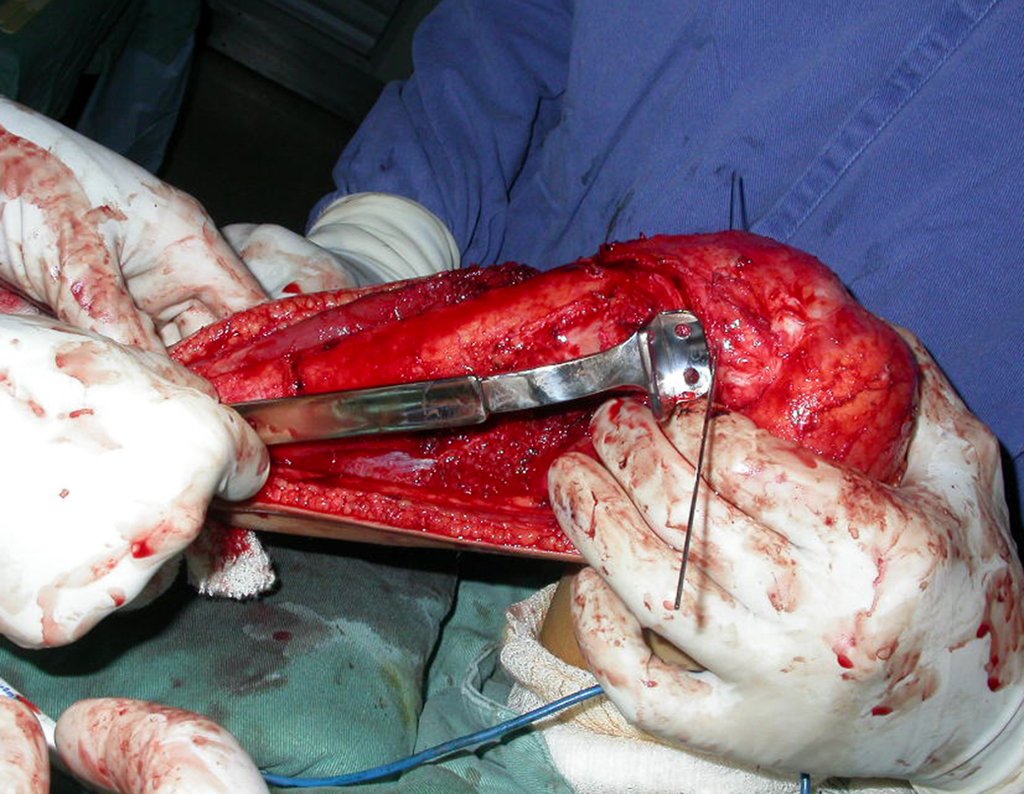
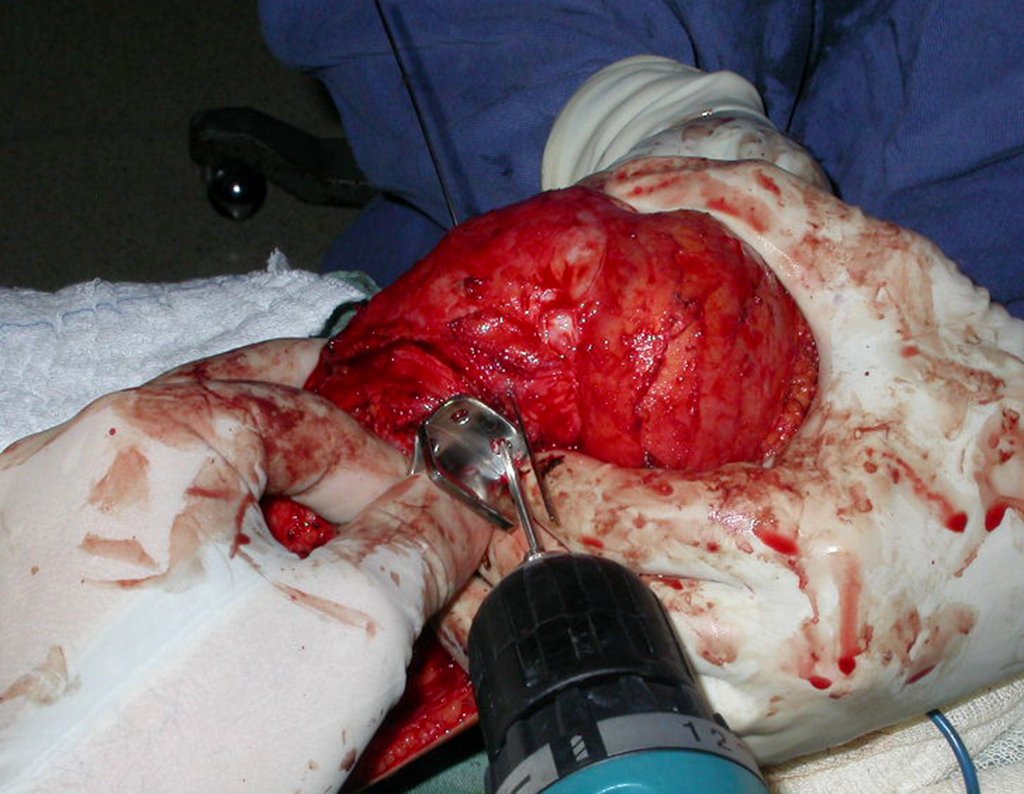
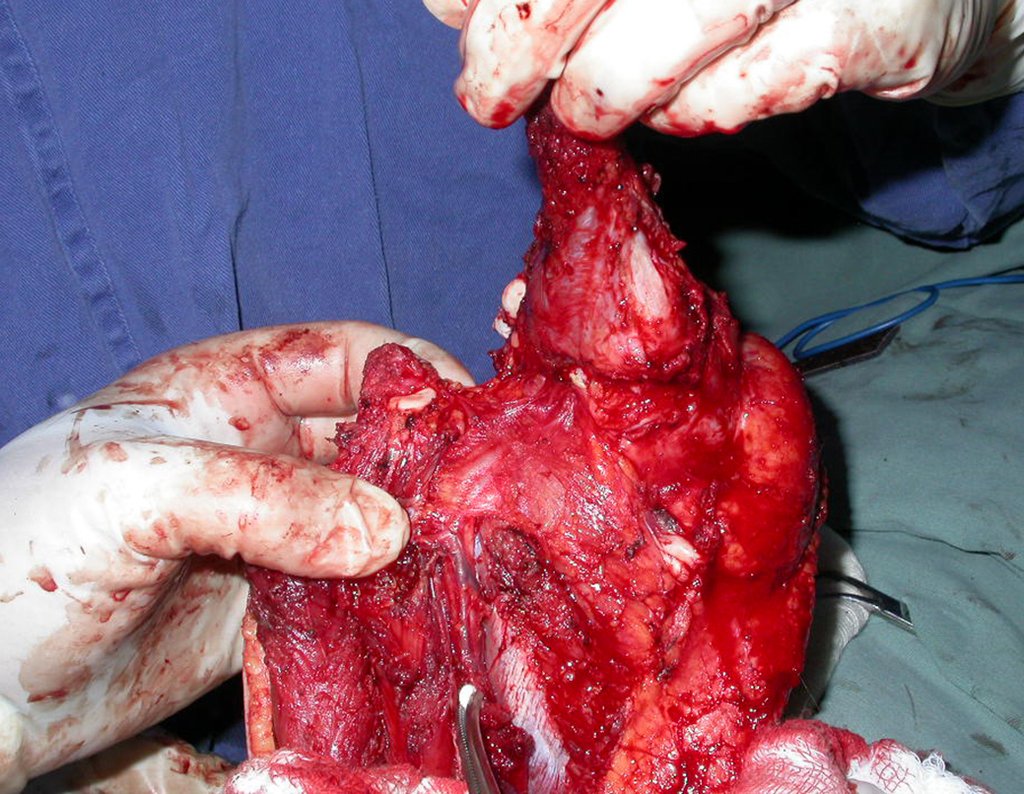
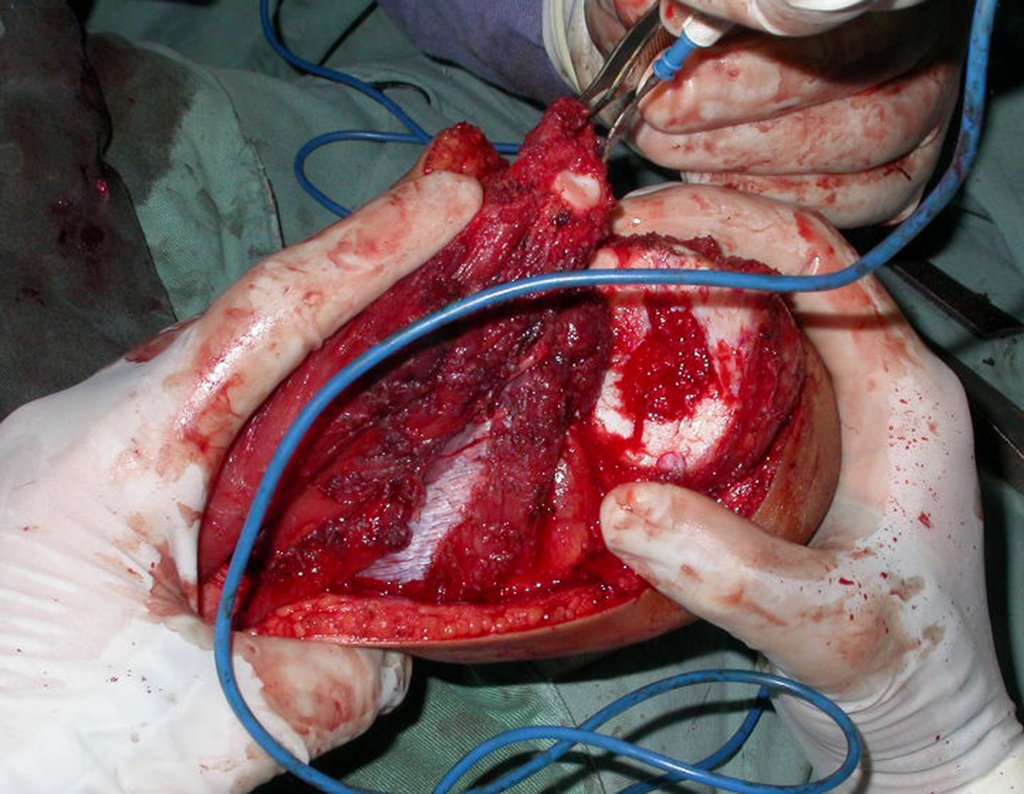
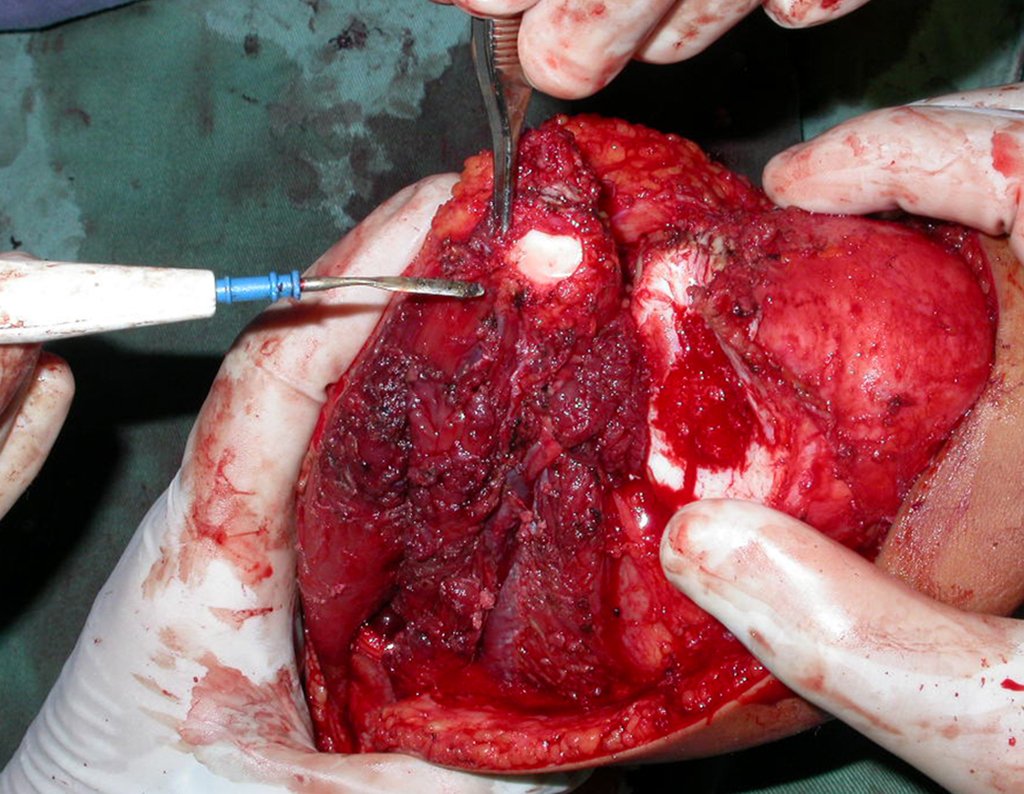
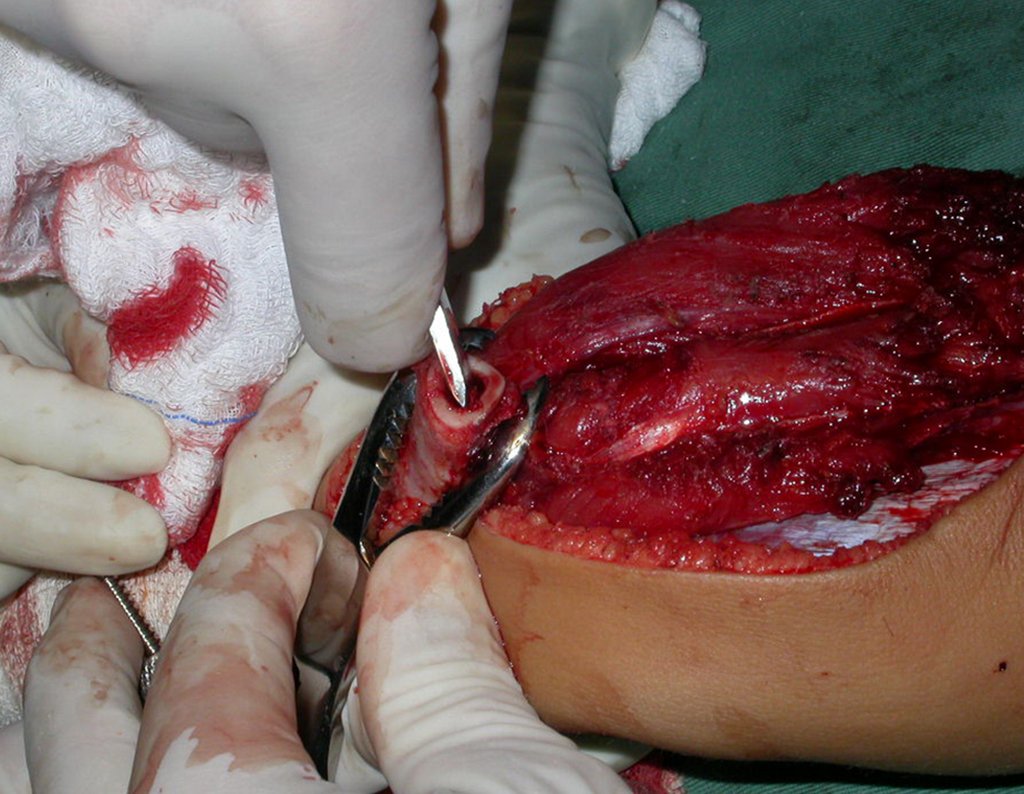
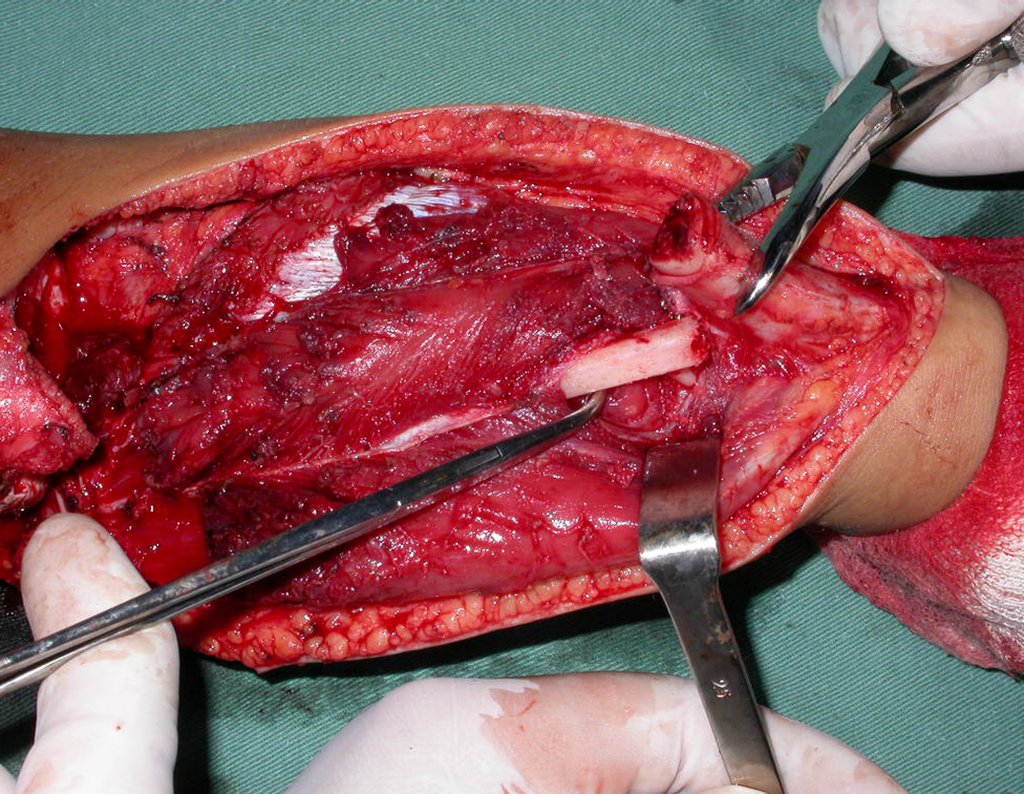
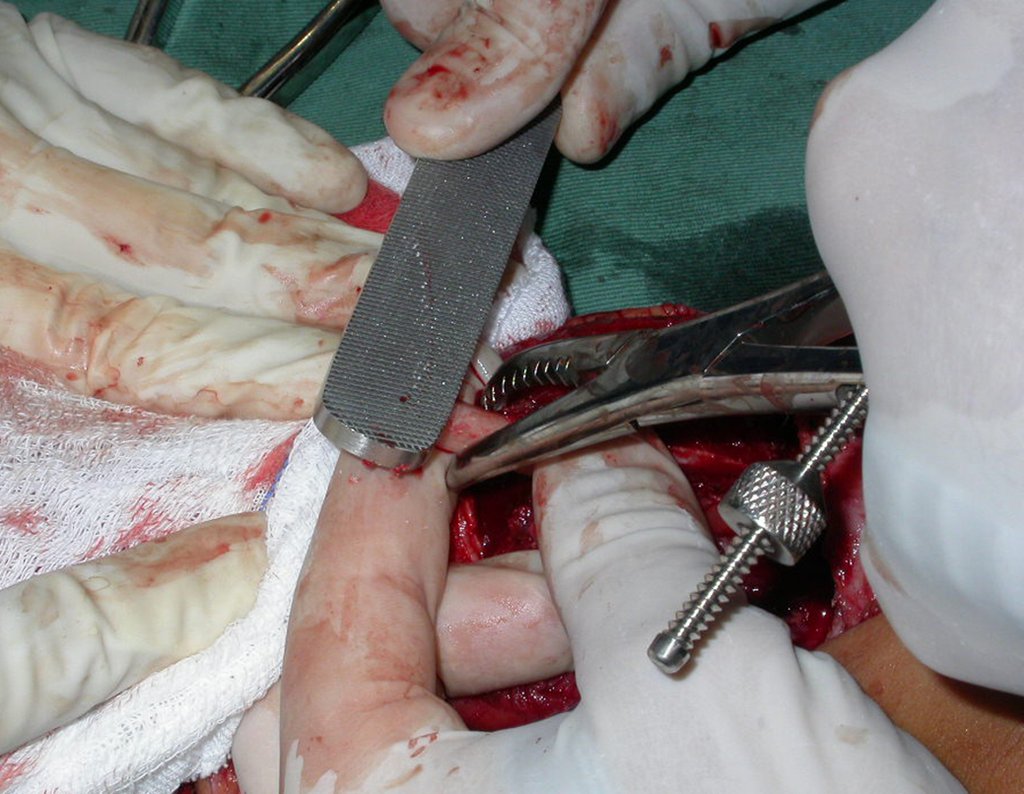
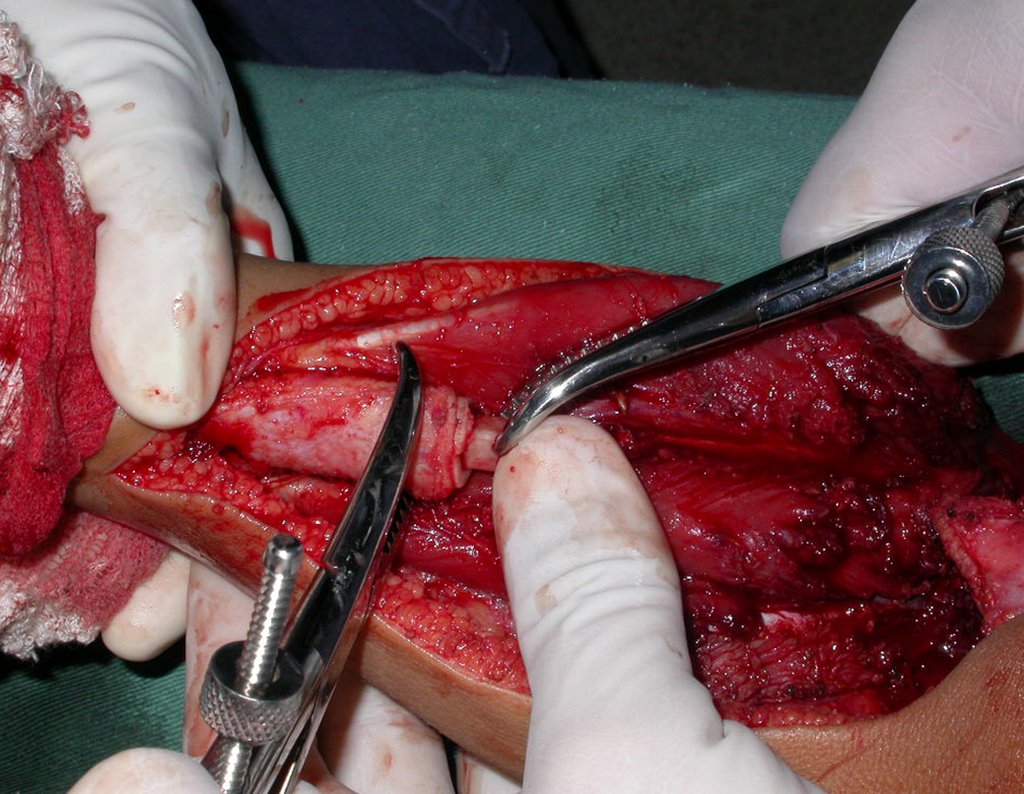
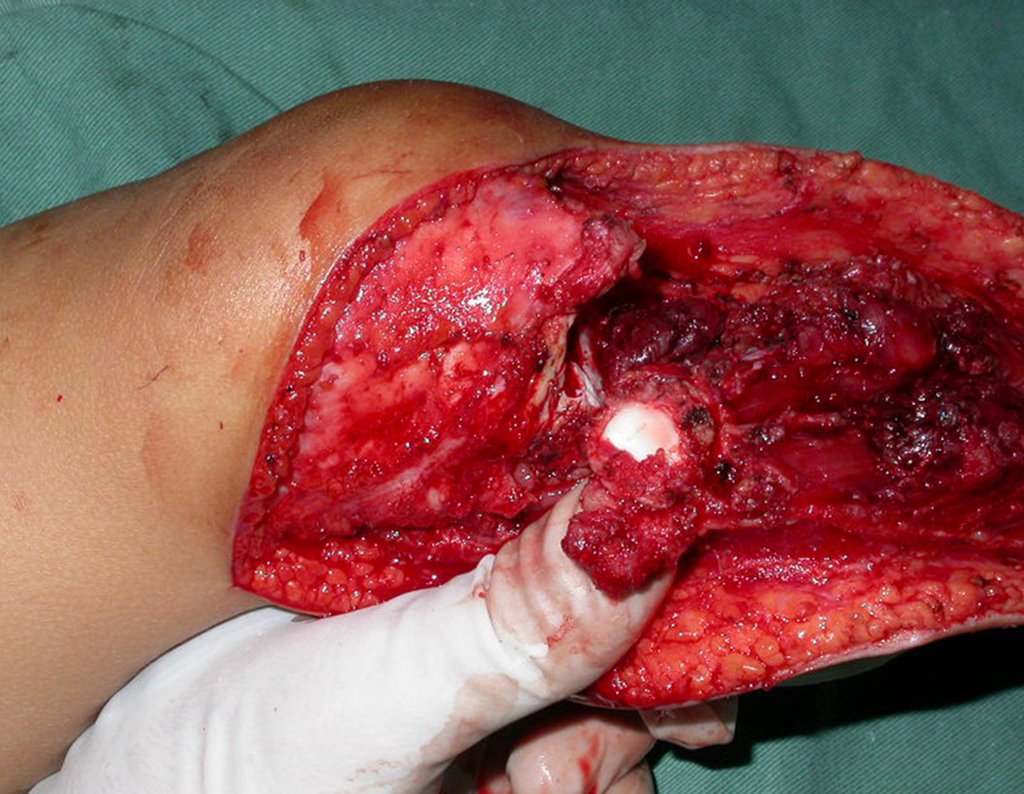
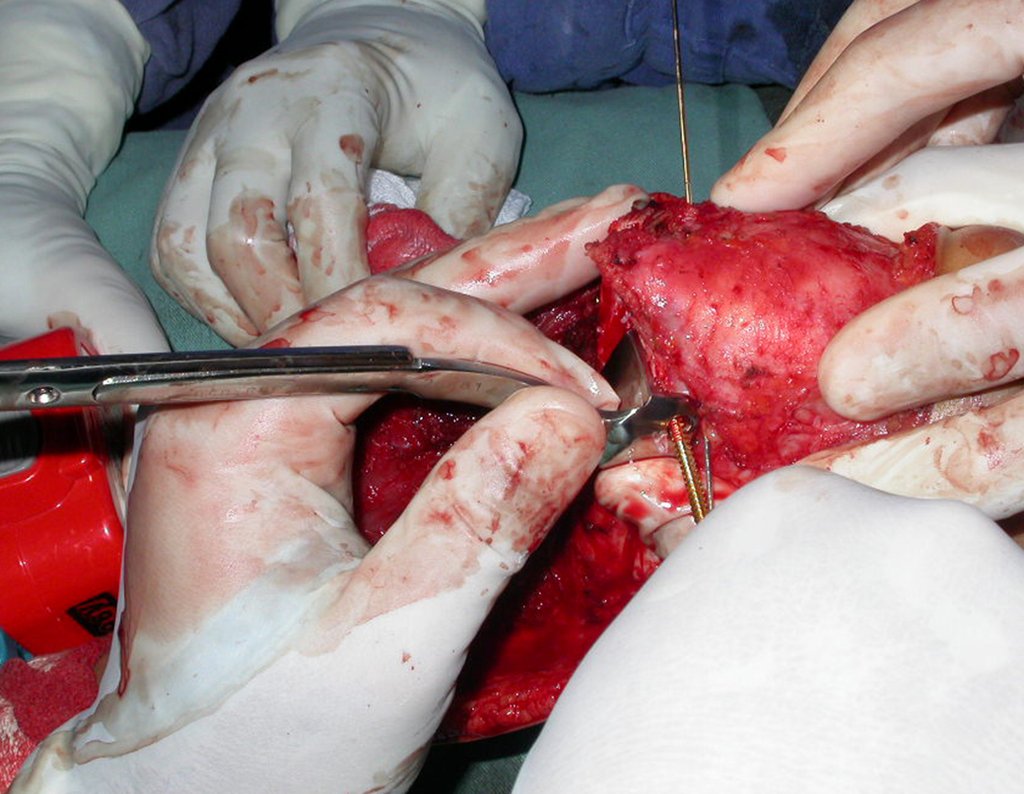
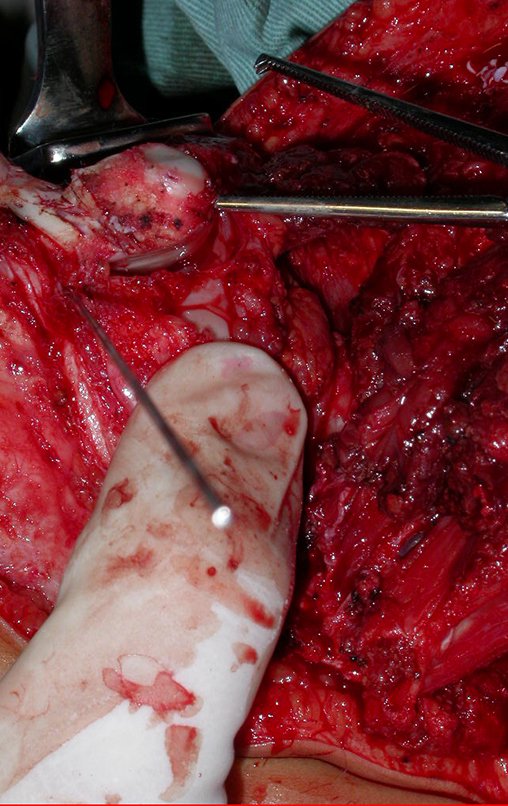
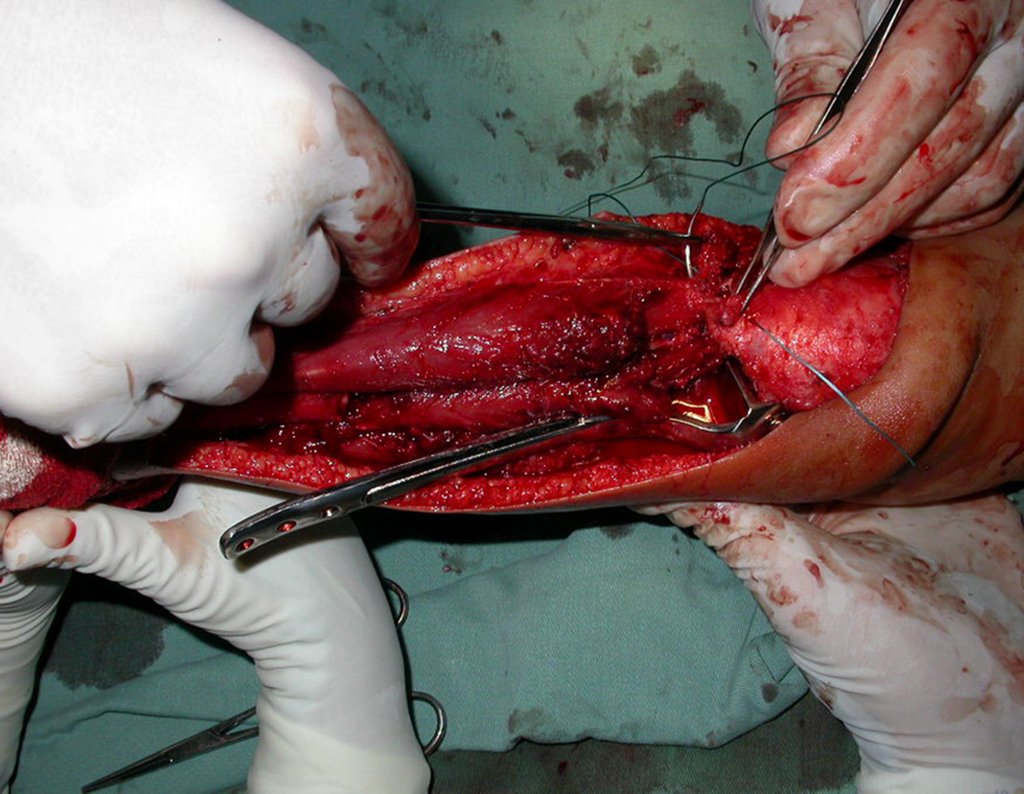
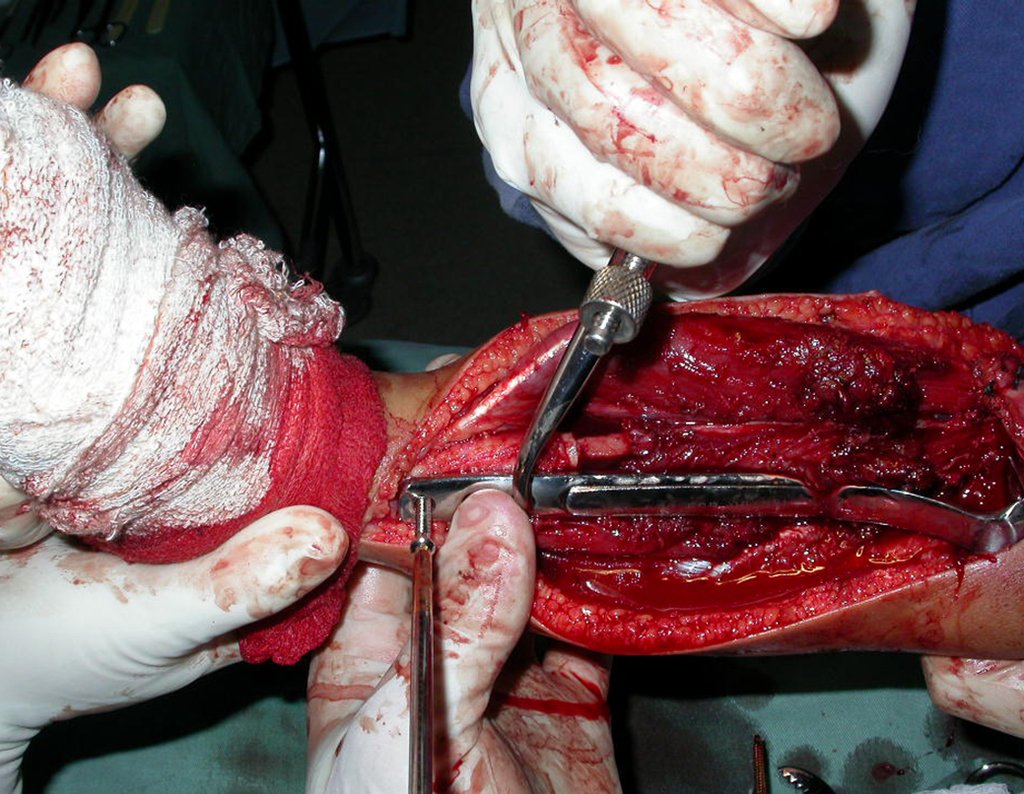
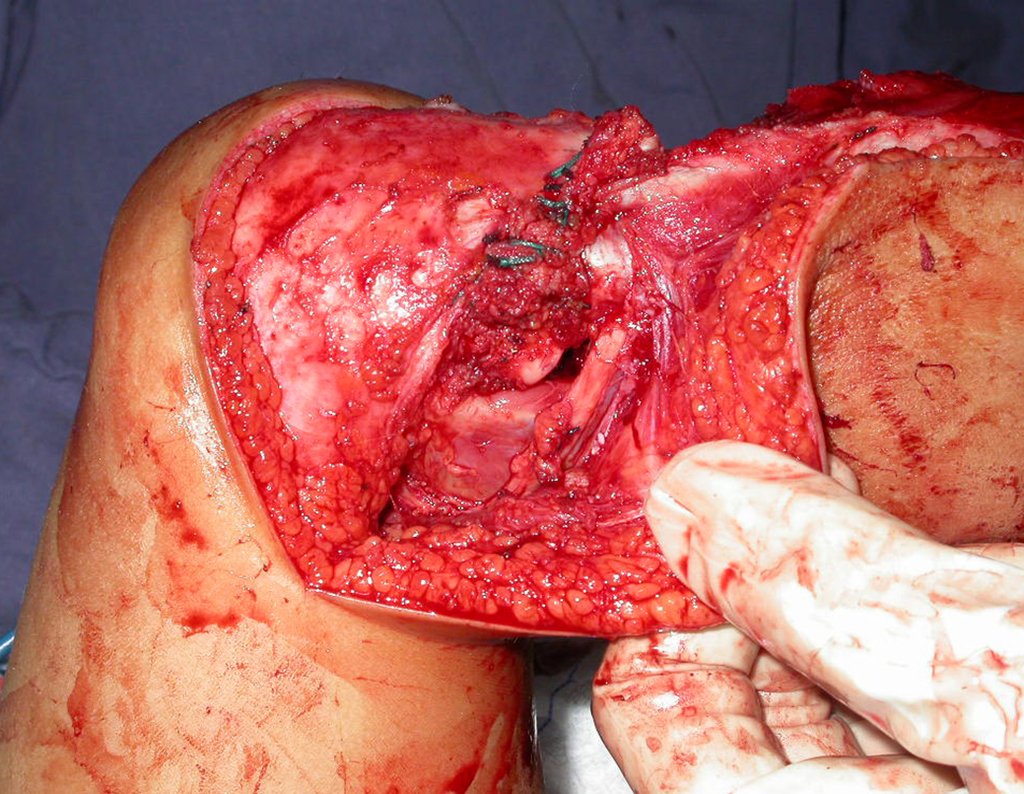
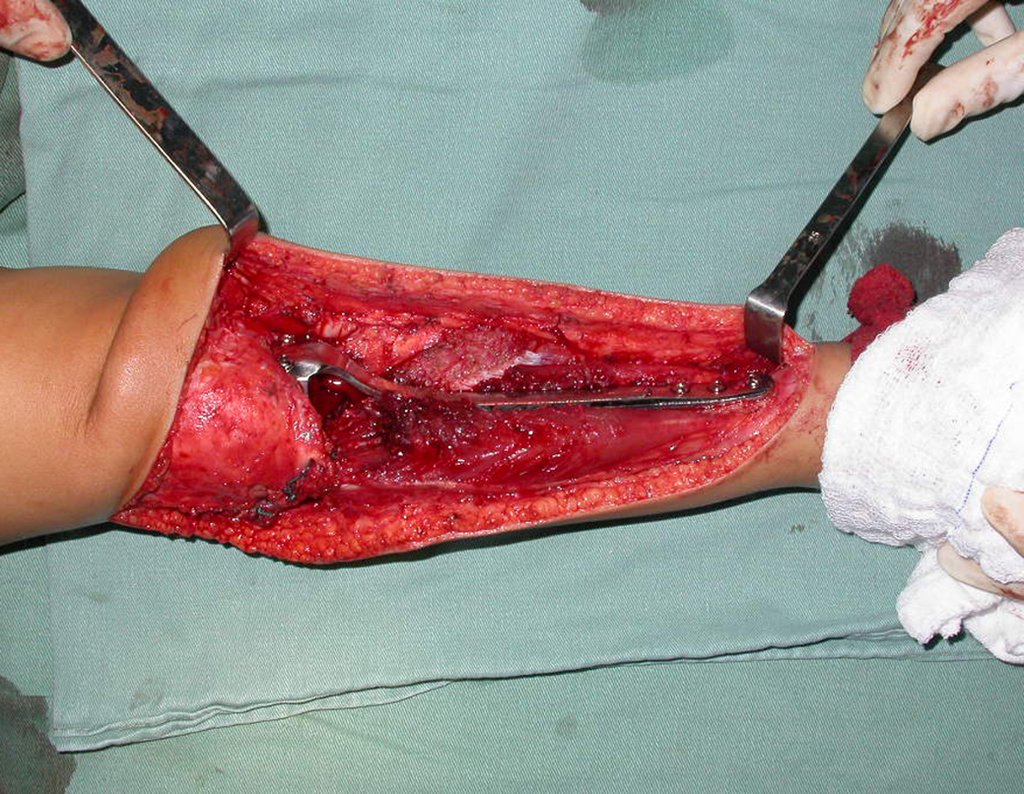
In December 2006, the patient underwent surgery to resect the proximal metaphyseal segment of the tibia, including the growth plate, and self-transplantation of the growth cartilage of the proximal segment of the fibula, through transfer to the tibia, without microsurgery.
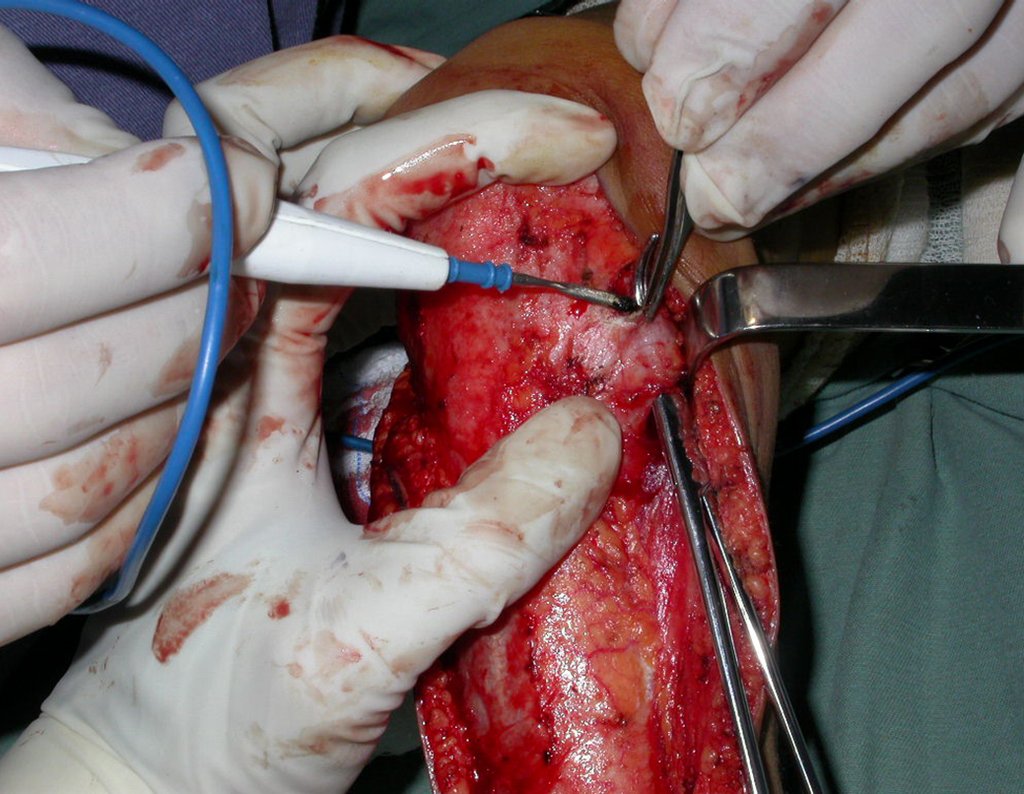
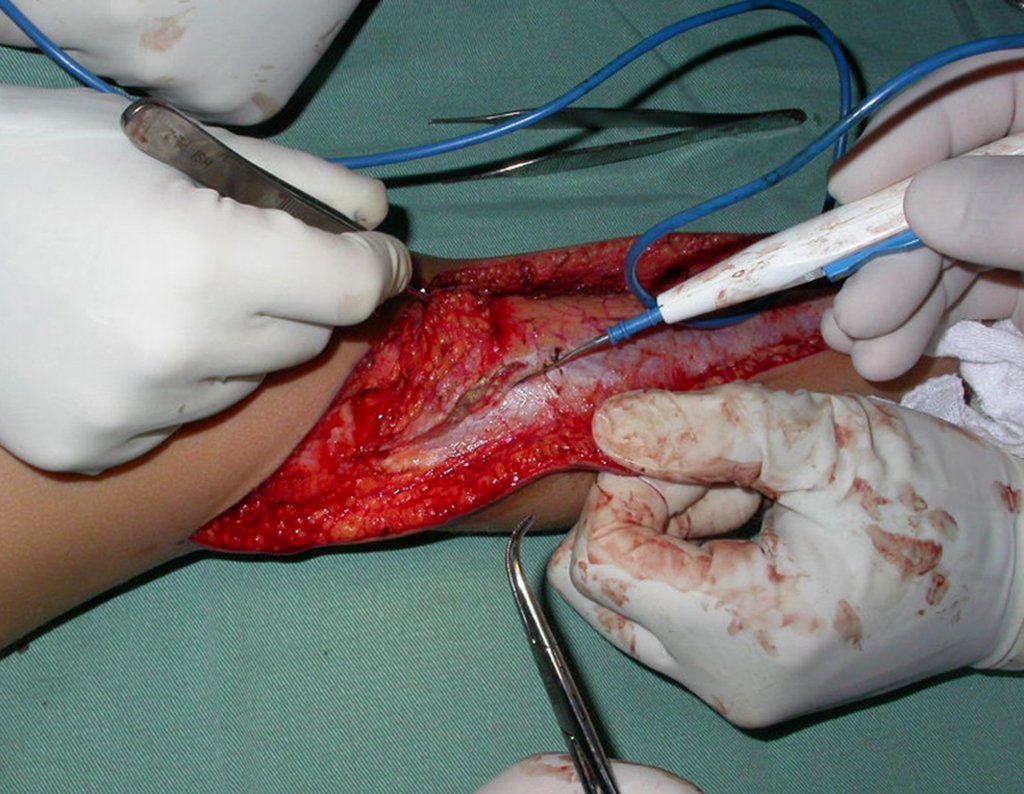
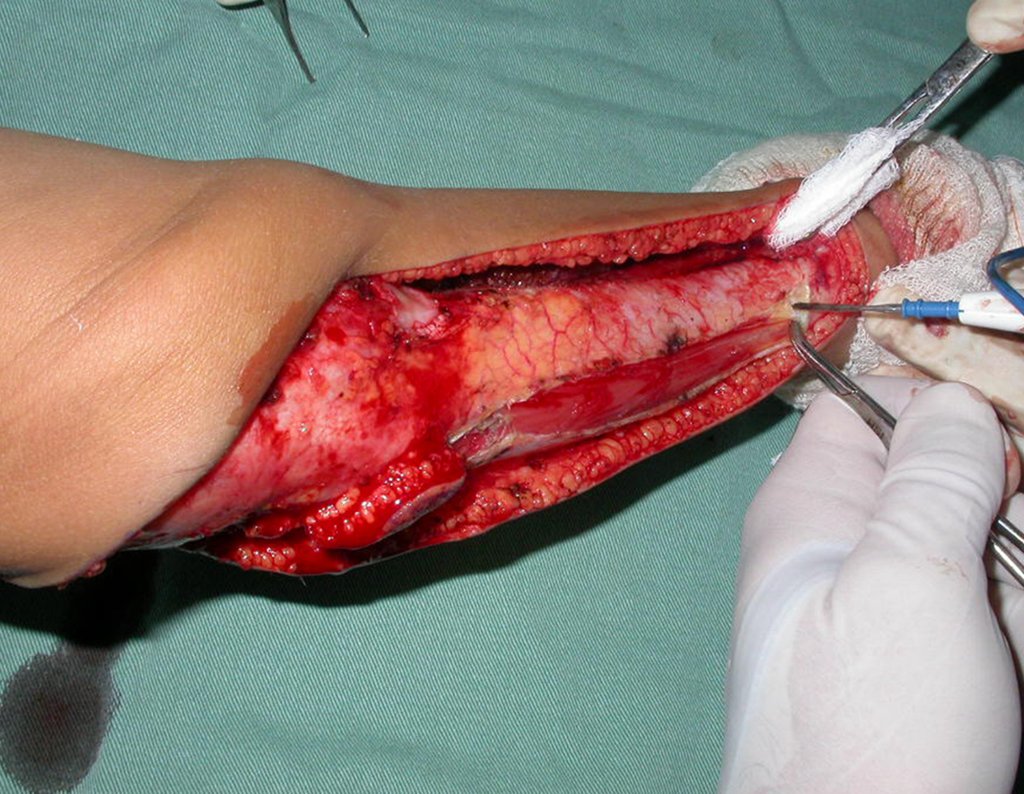
SURGICAL TECHNIQUE:
The patient is positioned in a horizontal supine position. A single, curved access route is used, starting above the proximal tibio-fibular joint, descending and curving medially towards the crest of the tibia and continuing distally along the internal surface of the tibia, until a few centimeters below the place where fibular osteotomy will be performed.
Video 3: On 02/12/2007, patient showing good movement of his right leg, six weeks after surgery.
Video 4 : Function of the knee operated on 04/12/2007, four months after surgery.
Video 5 : Walking on 05/14/2007, five months after surgery, undergoing adjuvant chemotherapy.
Video 6 : Patient undergoing chemotherapy, limping due to angular deviation, due to non-union of the proximal end of the fibula, on 09/26/2007, nine months after surgery.
Video 7 : Patient walking six months after the femoral fracture, waiting for the end of chemotherapy for reoperation.
Video 8 : Knee function, one and a half years after leg surgery and six months after the femur fracture.
Authors of the case
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com