Chondrosarcoma of the Femur
Intralesional curettage can be used in some cases of aggressive benign lesions, such as GCT (giant cellular tumor). However, a small incision cannot be used in any situation. When the curettage technique is indicated, we must have a broad view of the entire cavity and perform local adjuvant therapy, when necessary.
In this specific case, curettage is not indicated for the treatment of this lesion, much less with a small incision. The biopsy suggested the diagnosis of chondroma, but it was a grade II chondrosarcoma, which was the definitive diagnosis of the cured material.
With the diagnosis of malignant neoplasm and the “recurrence” condition, amputation of the limb was indicated. The patient does not accept the treatment and seeks us for a second opinion.
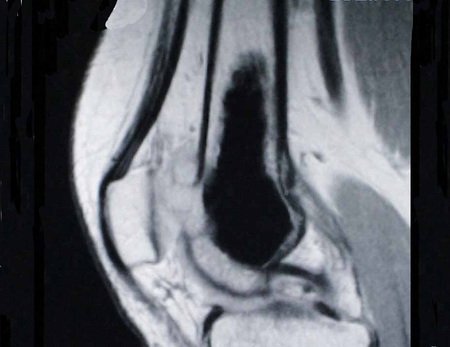
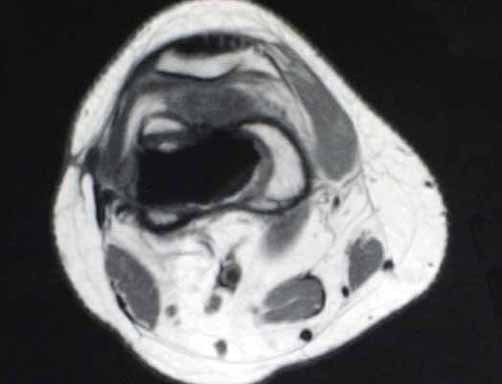
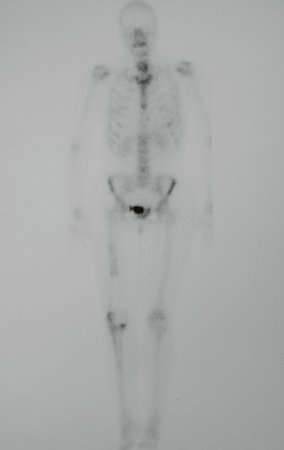
We can observe the presence of a remaining tumor in the immediate postoperative radiographs. The resonance images detail this situation (Figures 5 – 10)
We analyzed that, despite inadequate manipulation, we were facing a slowly evolving neoplasm and that we could attempt a wide resection of the affected region and reconstruct it with a non-conventional endoprosthesis.
If the study of the specimen did not reveal dedifferentiation, we could perform post-operative clinical and imaging controls every three months initially, and only perform the alternative of amputation if there was a recurrence after this wide resection.
We resected the distal third of the femur that was compromised, through a wide incision, seen in Figures 11 and 12 and documented in the radiographs of the prosthesis, Figures 13 and 14.
Authors of the case
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com