Extendable internal fixation device
INTRODUCTION
The search for biological solutions that make it possible to resolve bone defects, caused by locally aggressive tumor or pseudotumor lesions, congenital malformations, traumas and infections, has increasingly aroused the interest of orthopedists(1).
Advances in therapeutic resources in the treatment of malignant bone tumors have provided greater survival and even the prospect of a cure for patients. On the other hand, there is the inherent complication of endoprostheses over time. The correlation of these factors therefore requires the improvement of biological reconstruction methods that aim to be definitive(1-4). Reviewing the literature regarding bone reconstructions in the developing skeleton, it can be seen that this subject is of current interest(1,2,4-6).
DESCRIPTION OF THE TECHNIQUE
In February 1999, the nine-year-old male LCAA patient was undergoing preoperative chemotherapy treatment for diaphyseal Ewing sarcoma of the right femur at the Pediatric Hematology and Oncology Service of the Department of Pediatrics and Child Care of Santa Catarina. Casa Misericórida de São Paulo.
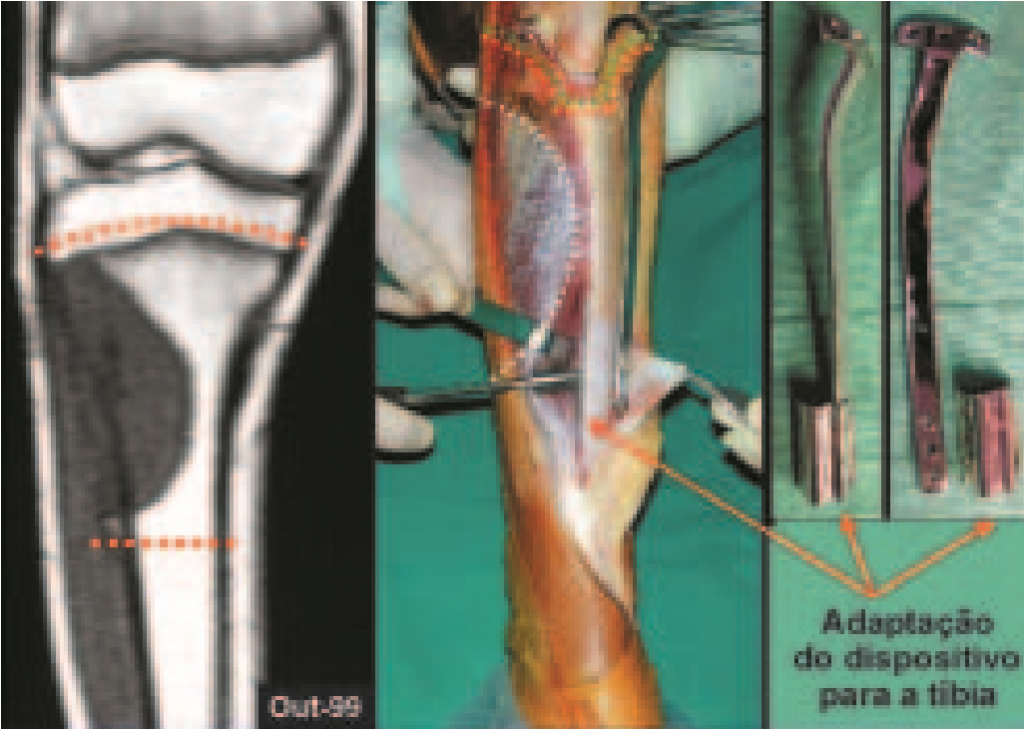

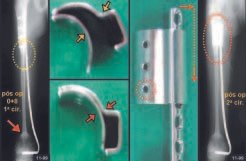
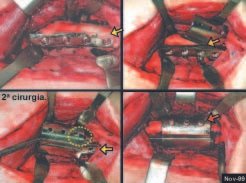
We currently use this device for immediately extensible internal fixation, and it currently consists of a single piece that has a curved side flap to adapt to the femur and humerus or it can be flat with an angle to adapt to the shape. triangular shape of the tibia (fig. 9). Another patient, WRC, 14 years old, with osteosarcoma of the right tibia, is a relatively recent example of reconstruction of the proximal metaphyseal segment of the tibia, with resection that also included the growth plate; We performed reconstruction with the fibula, including its epiphysis and using the epiphyseal plate of this fibula to provide growth (fig. 9). We can observe a slip of 0.75 cm by comparing the distances between the physeal plate of the transported fibula and the limit of the extensible device. Radiographic correction of the valgus inclination of the tibial plateau and clinical realignment of the knee can be seen (fig. 10). The patient is currently in the final phase of growth and has good knee function (Figs. 11 and 12).
COMMENTS
We believe that this device for extensible internal fixation, which we developed, can be used both for the treatment of selected cases of aggressive tumor lesions and also for other conditions, such as congenital malformations and sequelae of trauma or infections, which may require reconstructions that require a stabilization mechanism that allows the epiphysis to be fixed, but without blocking bone growth.
REFERENCES
1. Manfrini M., Gasbarrini A., Malaguti C., et al: Intraepiphyseal resection of the proximal tibia and its impact on lower limb growth. Clin Orthop 358: 111-119, 1999. 2. Eckardt JJ, Kabo JM, Kelley CM, et al: Expandable endoprosthesis reconstruction in skeletally immature patients with tumors. Clin Orthop 373: 51-61, 2000. 3. Capanna R., Bufalini C., Campanacci M.: A new technique for reconstructions of large metadiaphyseal bone defects. Orthop Traumatol 2:159-177, 1993. 4. Cool WP, Carter SR, Grimer RJ, Tillman RM, Walker PS: Growth after extendible endoprosthetic replacement of the distal femur. J Bone Joint Surg [Br] 79: 938-942, 1997. 5. Baptista PPR, Guedes A., Reggiani R., Lavieri RF, Lopes JAS: Tibialization of the distal fibula with preservation of the epiphyseal plate: preliminary report. Rev Bras Ortop 33: 841-846, 1998. 6. Baptista PPR, Guedes A., Reggiani R., Lavieri RF, Pires CEF: Tibialization of the fibula: description of the surgical approach. Rev Bras Ortop 33: 861-866, 1998.
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com