Chondroblastoma
Codman, in 1931, described it as a different form of manifestation of the “calcified giant cell tumor” of the proximal humerus. It was later found to be a tumor other than the gigantocellular tumor (GCT).
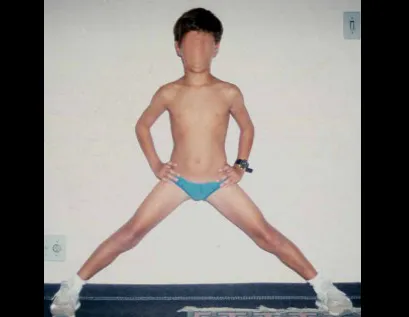
It preferentially affects the epiphysis of long bones, as a bone rarefaction lesion, with foci of calcification, in male patients, in the first and second decade of life, therefore with the growth plate open. Therefore, it affects the epiphyseal region of growing long bones (figs. 1 and 2) and, less frequently, the apophyseal portion (figs. 3 and 4).
This injury, as it occurs intra-articularly, can present a clinical picture similar to arthritis, when it causes reabsorption of the epiphysis (or apophysis), erosion of the cortical bone and joint invasion, leading to arthralgia, which can cause deformity and fracture and joint subsidence. It can, therefore, present local aggressiveness such as cortical erosion, growth plate erosion and joint invasion.
When there is radiographic manifestation of local aggressiveness, it is generally associated with areas of aneurysmal bone cyst. It presents differential diagnosis with simple bone cyst, aneurysmal, osteomyelitis, tuberculosis, arthritis, chondroma, giant cell tumor (osteoclastoma), early osteoid osteoma, pseudo-tumorous lesions, among others.
The treatment of chondroblastoma is surgical and must be carried out as soon as possible, as these lesions, despite being histologically benign, quickly progress to destruction of the local bone framework. It consists of intralesional curettage followed by local adjuvant (phenol, electrothermia, liquid nitrogen, etc.) and placement of a bone graft or cement (polymethylmethacrylate).
In very advanced lesions, segmental resection followed by placement of a prosthesis or arthrodesis may be necessary. The best indication to avoid local recurrence is segmental resection.
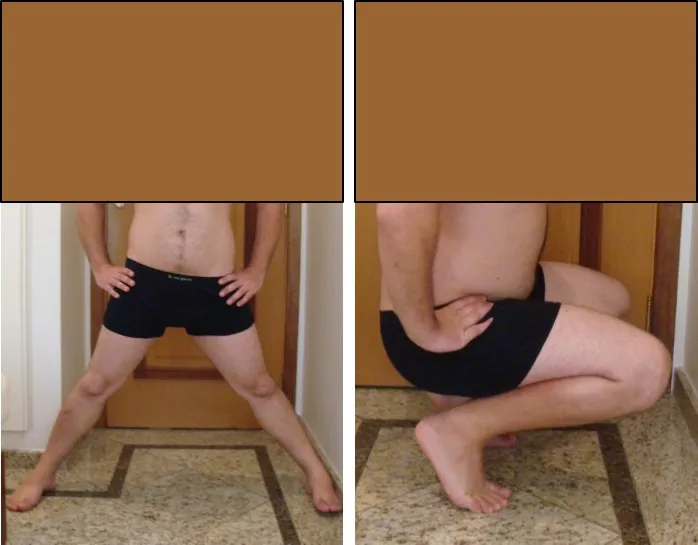
However, due to the articular location of the chondroblastoma, it is preferable to provide adequate surgical access to each region, as in this example, which affects the posteromedial region of the femoral head (fig. 5 and 6).
Currently, the patient is well and asymptomatic, 24 years after surgery for the femoral injury and 22 years after the removal of some of the metastatic nodules.
The prognosis can be guarded for both local recurrence and orthopedic complications such as joint degeneration and growth deficit.
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com