
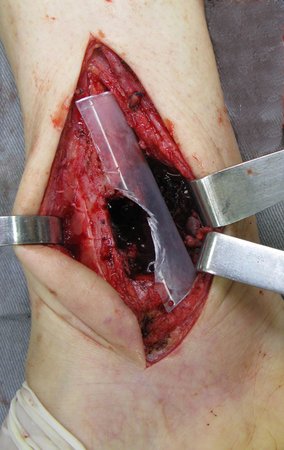
Bone metastasis from squamous cell cancer in the ankle

When we analyzed the images, we observed a well-defined lesion in the distal region of the right tibia, with sclerotic edges on the lateral surface, without destruction of the medial cortex and without periosteal reaction. We can imagine that this area represents a lesion of low aggressiveness and likely benign origin. However, we cannot forget that we are not facing an examination finding, that is, the injury is causing symptoms of pain, which led the patient to complain to her doctor. Furthermore, his history of two neoplasms creates the need to rule out or confirm the metastatic etiology of this lesion.
The next step in managing this case is to perform a complete tumor staging. We request tomography scans of the thorax, abdomen and pelvis to search for other neoplasms in parenchymal viscera. We did not find other tumor sites. We request a total body bone scan to check for other skeletal injuries. This exam, which is very sensitive and not very specific, allows the investigation of other skeletal sites with possible neoplastic involvement, which did not reveal other affected sites other than the right ankle. Serum protein electrophoresis is mandatory to investigate multiple myeloma, another neoplasm compatible with the patient’s age that often presents bone lesions not visualized on scintigraphy. This patient did not present changes in electrophoresis. Magnetic resonance imaging of the ankle is necessary for local tumor staging and surgical planning.
The possibility of it being a primary bone tumor cannot yet be completely ruled out. Academically, the best approach would be a biopsy of the ankle with the aim of differentiating a sarcoma, which would represent a primary tumor, from a carcinoma that would confirm the metastatic origin of this lesion. We initially recommended percutaneous biopsy for this patient. However, between the first evaluation and the return, this patient presented a major destructive evolution of the ankle seen in this x-ray below, taken one month after the first. If we performed the biopsy and waited for the results to then plan a resection, this joint would probably be doomed by rapid tumor progression. At this moment, the patient is at high risk of a pathological bone fracture in the ankle, with a risk of collapse of the remaining bone architecture and severe local functional impairment. It has 11 points out of 12 according to the Mirrels classification, which predicts the risk of fracture in metastatic lesions.





Authors of the case
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com



























