Intramuscular Hemangioma of the Leg
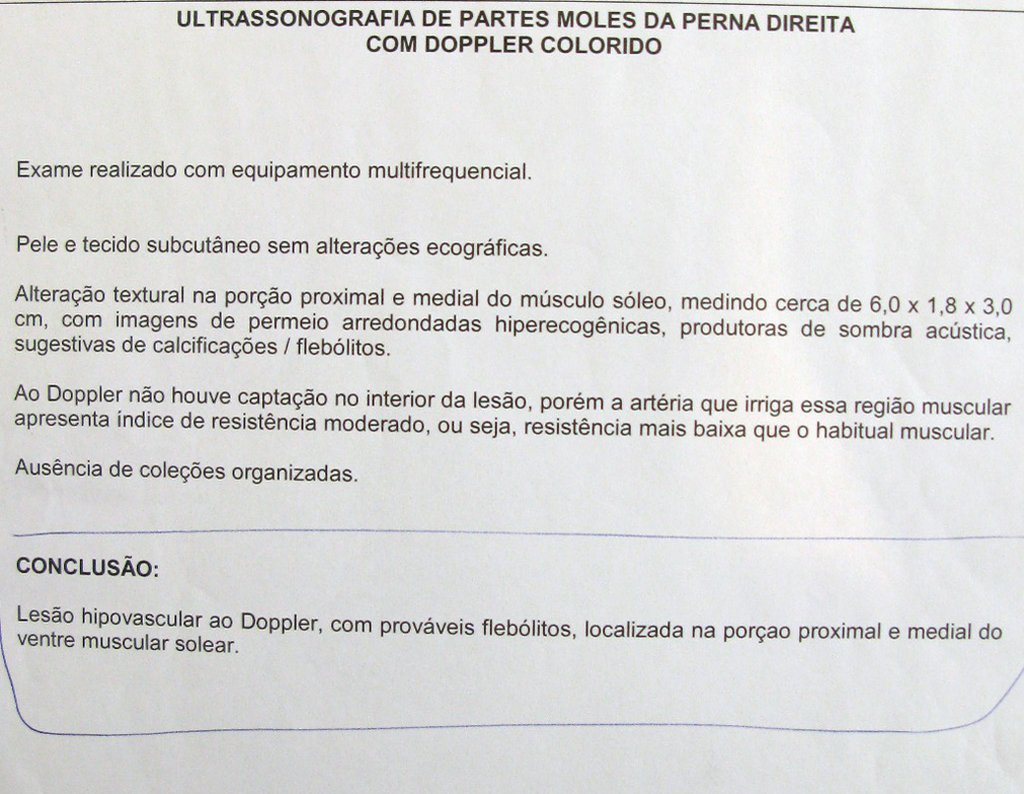
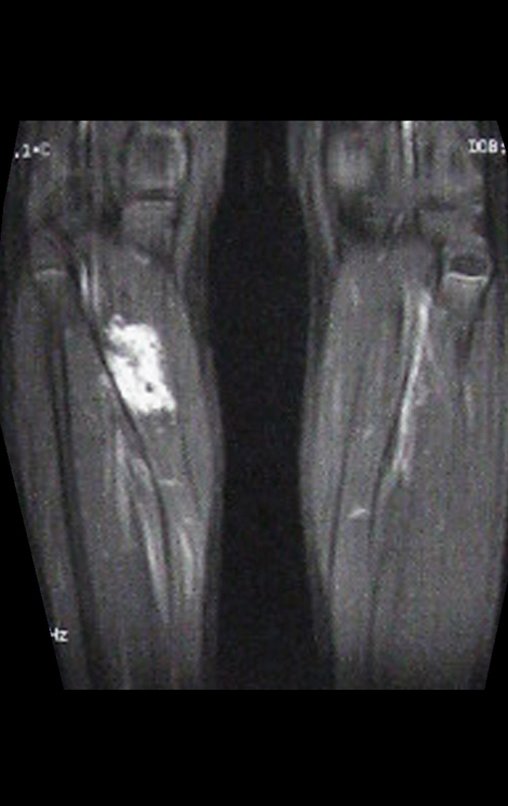
Intramuscular hemangioma. A 12-year-old male patient complains of pain in the right calf since he was eight years old, unrelated to trauma and progressively worsening over this period. He sought medical attention where he was diagnosed with “ growing pains ”. He was treated with painkillers and recommended rest, with no improvement in his condition. He took x-rays of the right leg, which, according to the patient’s mother, showed no changes.
Over the years, the pain complaint intensified and only improved with forced knee flexion or external compressive bandaging, performed by the patient himself. In the last six months the pain has become disabling, preventing walking. A palpable bulge appeared in the posterior region of the left leg, which reduced in size in the morning and increased at the end of the day. The patient reported a reduction in the volume of the palpable mass with elevation of the limb.
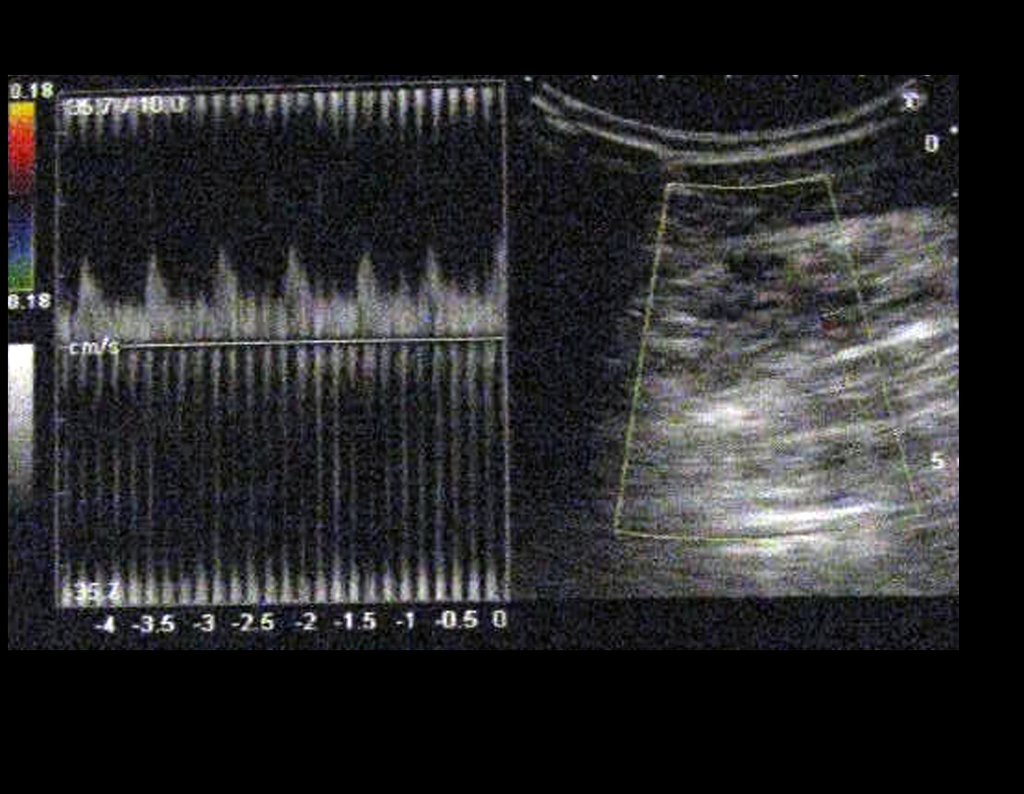
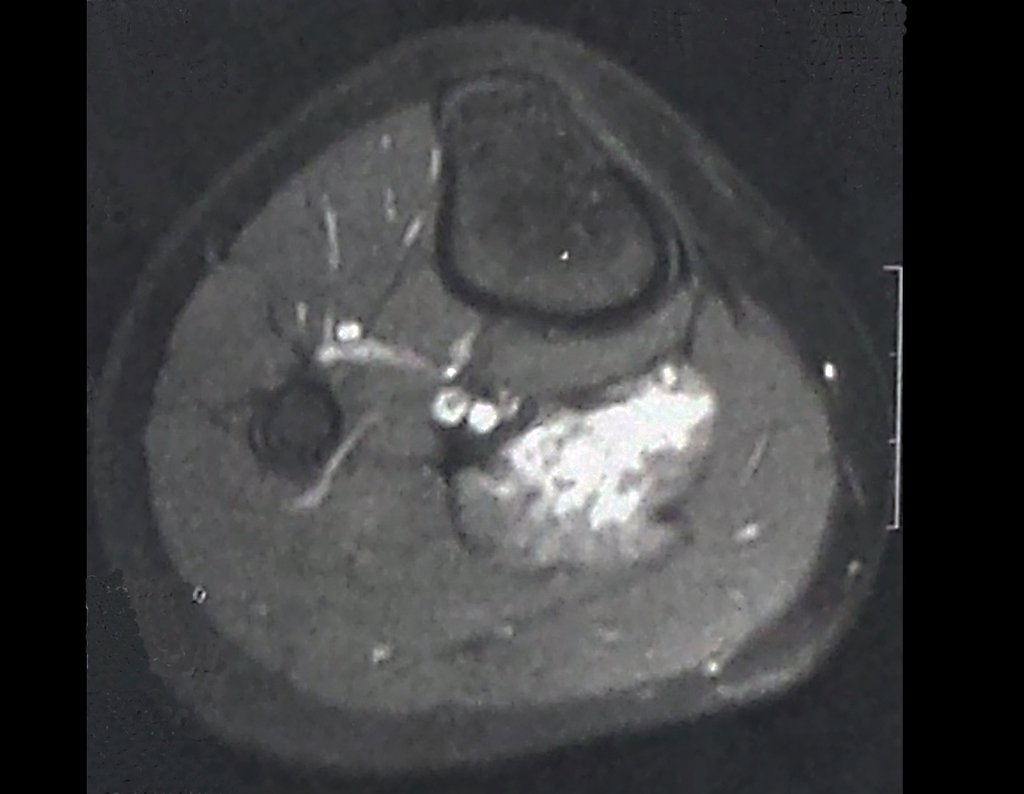
Hemangioma is a benign vascular tumor very similar to normal blood vessels. It can be difficult to distinguish between a hemangioma, a hamartoma (embryonic remnant) and a vascular malformation. It is most common in the skin and subcutaneous tissue. When it appears in the muscles, the lower limb is the most common. The presence of pain and edema associated with venous stasis is common.
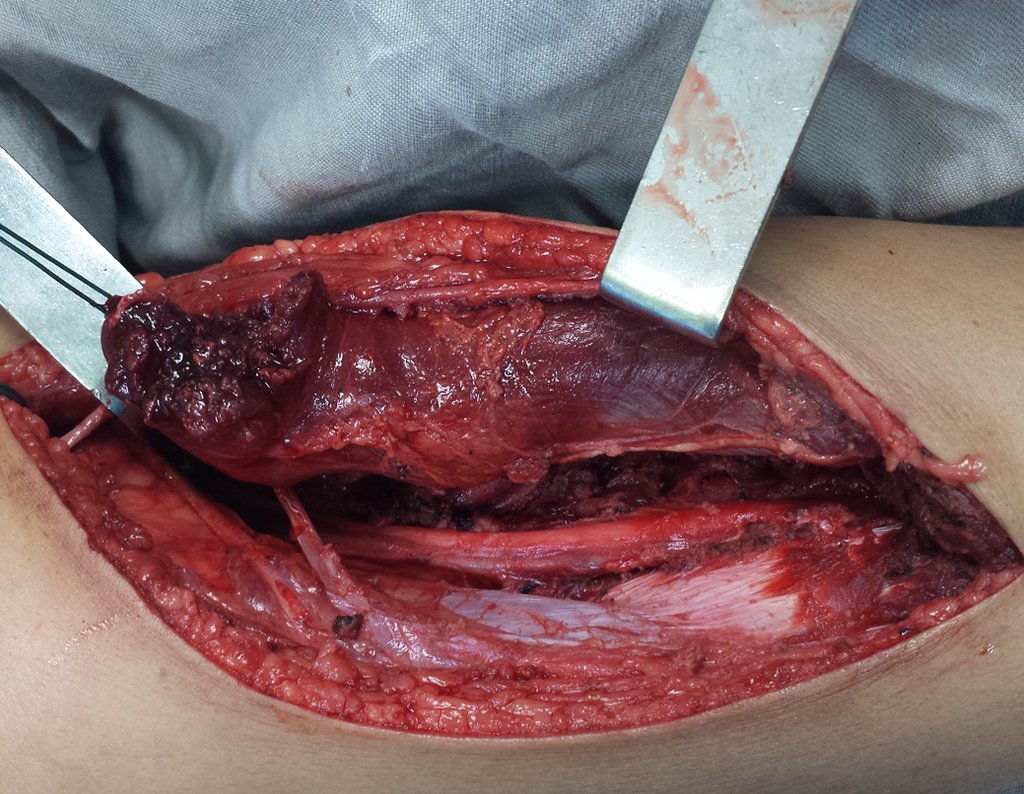
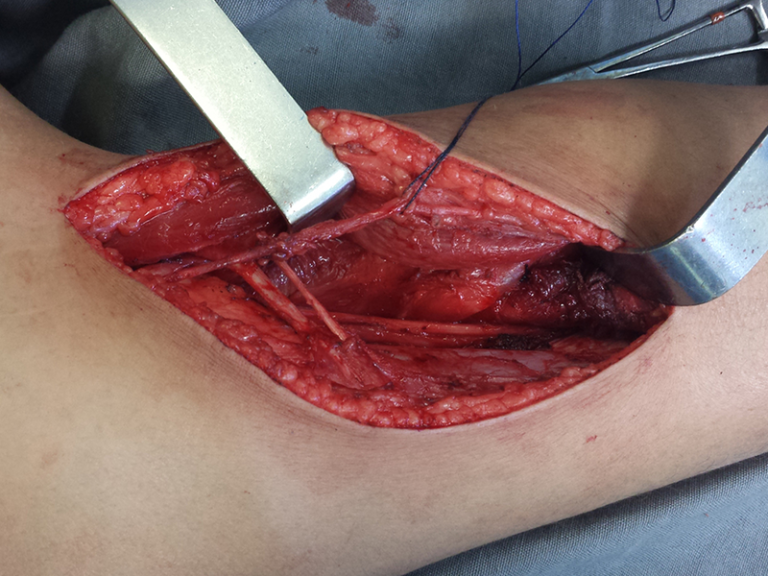
With this history, clinical picture and imaging characteristics, one can practically conclude the diagnosis of a vascular lesion, with a high probability of being an intramuscular hemangioma.
Given the patient’s disabling pain, surgical treatment to resect the lesion is justified, aiming to alleviate the symptoms. In this situation, the biopsy, despite confirming the histological diagnosis, may be dispensed with. As it is a highly vascularized lesion, a percutaneous biopsy could cause difficult-to-control bleeding, in addition to the possibility of an inconclusive diagnosis of normal vascular tissue.
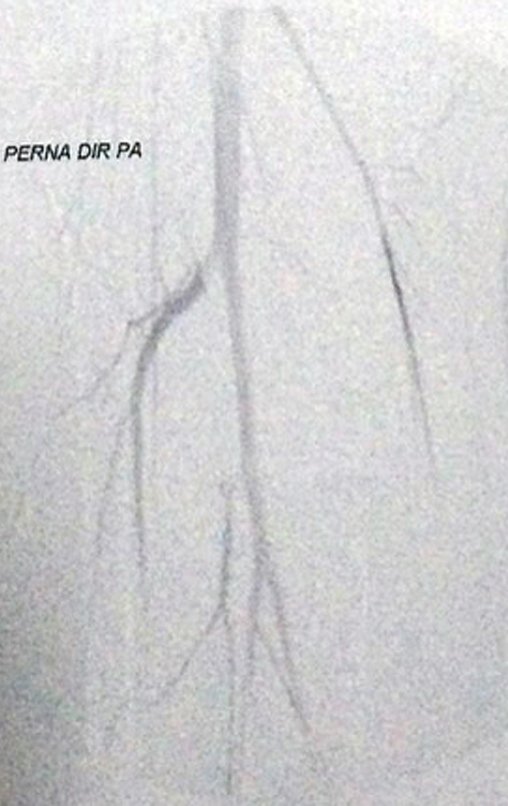
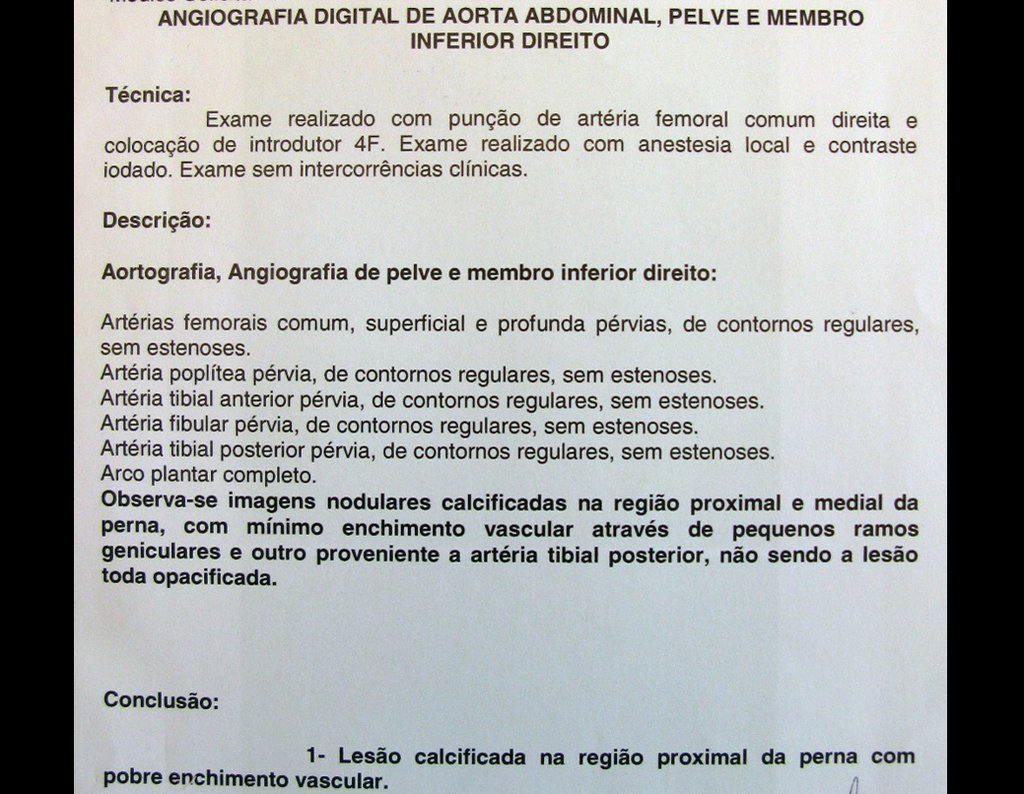
Arterial embolization is a form of control for some neoplastic lesions and can eventually be used before surgical resection, to reduce the size of the lesion, symptoms and intraoperative bleeding. In the case of hemangioma, embolization is limited because it is essentially a venous lesion, as confirmed by the preoperative angiography performed.
Video 1 : One month post-operative. Observe the reduction of the operated right calf, compared to the left. Despite resection of the medial belly of the gastrocnemius, we did not observe any functional deficit.
Case Author
Author: Prof. Dr. Pedro Péricles Ribeiro Baptista
Orthopedic Oncosurgery at the Dr. Arnaldo Vieira de Carvalho Cancer Institute
Office : Rua General Jardim, 846 – Cj 41 – Cep: 01223-010 Higienópolis São Paulo – SP
Phone: +55 11 3231-4638 Cell:+55 11 99863-5577 Email: drpprb@gmail.com